USMLE® Sample
Questions: Steps 1, 2 & 3
UWorld USMLE questions mirror the style and quality of the NBME, giving you the most authentic preparation for every step of the exam. Work through the sample questions below and experience the renowned answer explanations that strengthen understanding, sharpen reasoning, and build exam-day confidence.
Master the USMLE with Proven Exam-Style Questions
Learn by
Doing
Increase Your Confidence
Material You
Can Trust
Free USMLE Questions & Rationales - Try the UWorld Difference
A 3-month-old boy is evaluated for large-volume diarrhea and failure to thrive. The patient was born via spontaneous vaginal delivery at 38 weeks gestation. His mother reports that the pregnancy was uncomplicated and there is no family history of gastrointestinal disease. Physical examination shows mild abdominal distension, muscle wasting, and pitting edema. Histochemical evaluation reveals absence of enteropeptidase activity in the proximal intestinal villi. Activity of which of the following substances is most likely impaired in this patient?
- Amylase
- Bile salts
- Lactase
- Pepsin
- Secretin
- Trypsin
Explanation:
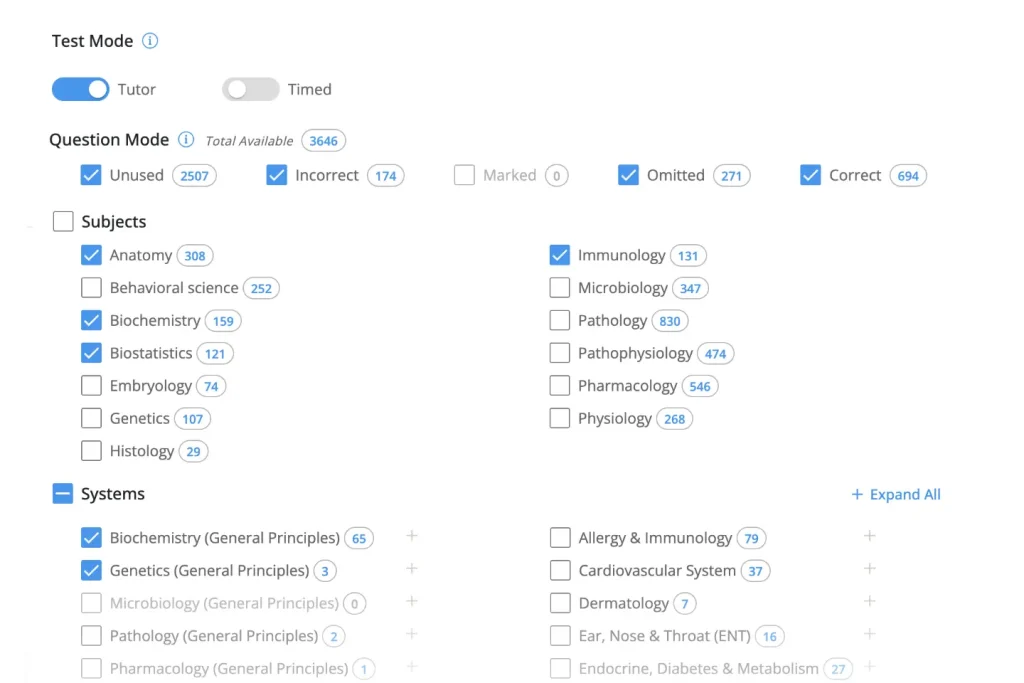
Although chemical digestion of proteins begins in the stomach, the majority of enzymatic breakdown and absorption occurs in the small intestine. Dietary proteins exist predominately as polypeptides; in order to be absorbed, they must be hydrolyzed to tripeptides, dipeptides, and amino acids. Hydrolysis begins in the stomach with the activation of pepsin by hydrochloric acid; it continues in the proximal small intestine, catalyzed by the pancreatic enzymes trypsin, chymotrypsin, carboxypeptidase, and elastase.
Pancreatic enzymes, including trypsin, are secreted in their inactive forms. Enteropeptidase, a duodenal brush border enzyme, is responsible for activation of trypsin from its inactive precursor, trypsinogen. Once active, trypsin functions to cleave peptide bonds in dietary proteins and activate the other pancreatic enzymes. Enteropeptidase deficiency leads to both protein and fat malabsorption as trypsin is required to activate enzymes required for both lipid and protein digestion. The disease causes diarrhea, failure to thrive, and edema (due to hypoproteinemia).
(Choice A) Amylase is produced by the salivary glands and pancreas; it catalyzes the hydrolysis of complex carbohydrates to simple sugars.
(Choice B) Bile salts are formed through bile acid conjugation with amino acids glycine and taurine. This increases their solubility, allowing them to aid in lipid digestion and absorption through the formation of micelles.
(Choice C) Lactase is produced by the intestinal brush border and is responsible for the hydrolysis of lactose to glucose and galactose. Lactase non-persistence commonly develops during mid-childhood, resulting in lactose intolerance.
(Choice D) Chief cells of the stomach release the inactive form of pepsin, pepsinogen. Exposure to hydrochloric acid in the stomach activates pepsin, initiating protein digestion.
(Choice E) Secretin is a peptide hormone secreted by the S cells of the duodenum; it stimulates the secretion of bicarbonate from the pancreas and inhibits gastric acid secretion in the stomach. Neutralization of the acidic pH of food entering the duodenum from the stomach is necessary for the proper function of pancreatic enzymes.
Educational objective:
The duodenal brush border enzyme enteropeptidase activates trypsin from its inactive precursor, trypsinogen. Trypsin degrades complex polypeptides to dipeptides, tripeptides, and amino acids while activating other pancreatic enzymes. Enteropeptidase deficiency impairs both protein and fat absorption, leading to diarrhea, failure to thrive, and hypoproteinemia.
A 73-year-old man comes to the emergency department with unstable angina. He undergoes coronary angiography via the femoral approach. A stent is placed in the right coronary artery, and the patient is discharged. He returns to the emergency department 2 days later with blue discoloration of his right toe. He has pain and mild tingling in the affected toe. Medical history is significant for hyperlipidemia and coronary artery disease. On physical examination, the right toe appears cyanotic, and there is livedo reticularis affecting the right thigh. Peripheral pulses in the lower extremities are bilaterally palpable. Serum creatinine is 2.8 mg/dL (preoperatively it was 1.0 mg/dL). Which of the following histopathologic findings would most likely be seen on biopsy of this patient’s kidney?
- Cholesterol clefts in arterial lumen
- Glomerular crescent formation
- Hyperplastic arteriolar changes
- Extensive necrosis of proximal tubular cells
- Tubular obstruction with urate crystals
Explanation:
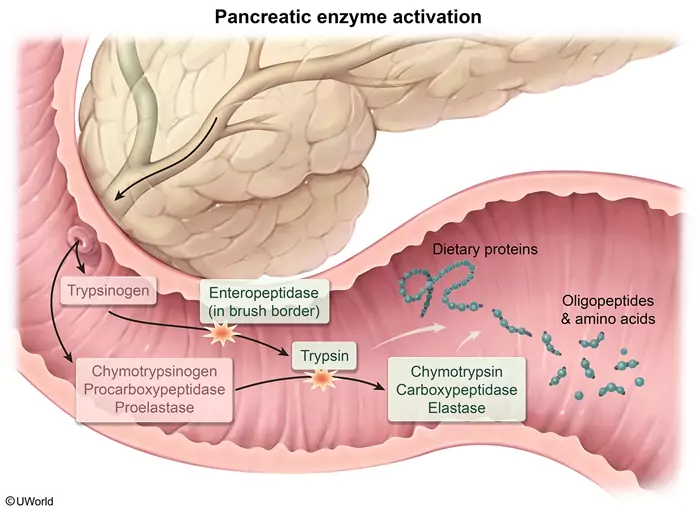
This patient has livedo reticularis, a blue toe, and acute kidney injury following coronary angiography; this presentation is concerning for atheroembolic disease. Invasive vascular procedures (eg, angiography, angioplasty, aortic surgery) can cause cholesterol-containing debris from atherosclerotic plaques to become dislodged from large arteries (eg, the aorta during cardiac catheterization) and shower microemboli into the circulation. These lodge in small, distal arterioles, resulting in ischemia of the corresponding organs and tissues; symptoms develop within a few days or weeks after the procedure. Skin findings (eg, livedo reticularis, blue toe syndrome) are the most common presenting signs. Pulses typically remain palpable as larger arteries are unaffected.
Signs of acute kidney injury (eg, oliguria, azotemia) are common in the setting of postprocedure atheroembolism and are frequently seen in elderly patients with preexisting renal atherosclerosis. Frank infarction with flank pain and hematuria does not occur due to the small size of the emboli. Cholesterol is dissolved during tissue preparation for microscopic evaluation, leaving the needle-shaped clefts that partially or completely obstruct the arcuate or interlobular renal arteries. Other organs that may be involved are the gastrointestinal tract and the CNS, including the retinal vessels.
(Choice B) Glomerular crescent formation is characteristic of rapidly progressive glomerulonephritis (RPGN). All forms of RPGN have an insidious onset with hematuria, hypertension, and edema.
(Choice C) Hyperplastic arteriolar changes (intimal fibroelastosis) are diagnostic of hypertensive nephropathy seen in patients with poorly controlled hypertension.
(Choice D) Atheroemboli only partially occlude the renal vessels, therefore acute tubular necrosis (ATN) does not typically occur early in the disease process. Complete vessel occlusion with resultant ATN can occur later (weeks to months) due to an endothelial inflammatory response. However, as opposed to toxin-induced ATN (eg, aminoglycosides), which causes diffuse, extensive proximal tubular injury, ischemic ATN typically causes patchy necrosis of the proximal tubules.
(Choice E) Urate nephropathy due to tubular obstruction from urate crystal deposition is usually seen in individuals with acute hyperuricemia (eg, tumor lysis syndrome). The classic presentation is acute renal failure during chemotherapy for a malignancy.
Educational objective:
Invasive vascular procedures can be complicated by atheroembolic disease, which may involve the kidneys, gastrointestinal tract, CNS, and the skin. Light microscopy shows a partially or completely obstructed arterial lumen with needle-shaped cholesterol clefts within the atheromatous embolus.
Physiologists are studying the forces governing glomerular ultrafiltration using a single nephron in an intact kidney of an experimental animal. Hydrostatic pressure in the glomerular capillary and Bowman space is measured using micropipette transducers. Colloid osmotic pressure in the glomerular capillary is estimated using the difference in plasma protein concentration in the afferent and efferent arterioles. The glomerular surface is assumed to be functionally intact with negligible filtration of plasma proteins into the Bowman space. From the data obtained, net filtration pressure is calculated at 10 mm Hg. A substance is instilled into the renal artery, and measurements are repeated. The net filtration pressure after the intervention is 20 mm Hg. Which of the following substances was most likely used in this experiment?
- Albumin concentrate
- Alpha-adrenergic agonist
- Angiotensin II agonist
- Prostaglandin inhibitor
- Vasopressin 2 antagonist
Explanation:
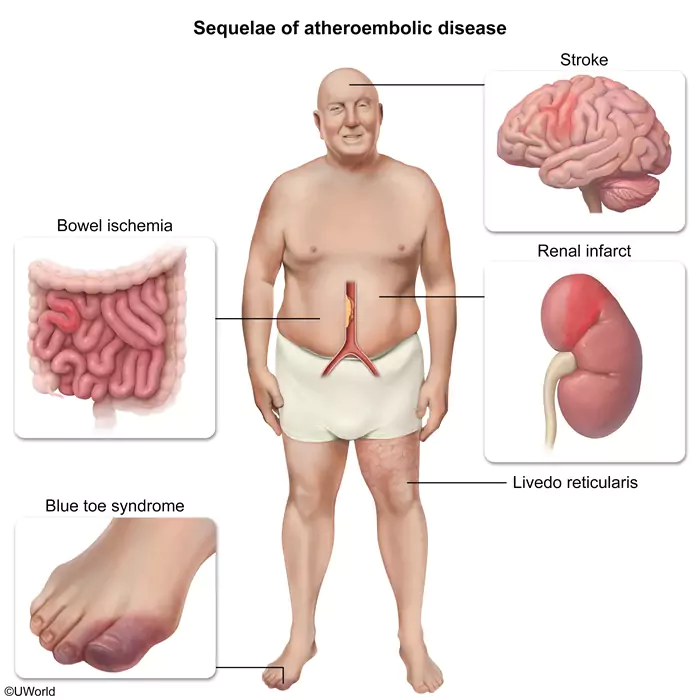
The net filtration pressure is a result of pressure gradients formed by Starling forces and is calculated by subtracting the oncotic pressure gradient from the hydrostatic pressure gradient (ie, net filtration pressure = [Pc − Pi] − [πc − πi]):
- The hydrostatic pressure gradient (Pc − Pi) is the difference between the hydrostatic pressure in the intraglomerular capillaries and Bowman’s space. Hydrostatic pressure in the capillaries is higher than in Bowman’s space, and provides the driving force for fluid efflux from the capillaries.
- The oncotic pressure gradient (πc − πi) is the difference between the oncotic pressure in the intraglomerular capillaries and Bowman’s space. Oncotic pressure is driven chiefly by large plasma proteins (eg, albumin), which do not freely filter across the glomerular capillary basement membrane due to both a size and a charge barrier. The high oncotic pressure in the capillaries counteracts the capillary hydrostatic pressure and decreases net fluid efflux from the capillaries.
This patient’s net filtration pressure has increased from 10 to 20 mm Hg after infusion of a substance. Increased net filtration pressure occurs due to either an increase in the hydrostatic pressure gradient or a decrease in the oncotic pressure gradient. Of the available options, only an angiotensin II agonist would increase the net filtration pressure. Angiotensin II preferentially constricts the efferent arteriole, resulting in an increased hydrostatic pressure gradient and increased net filtration pressure.
(Choice A) Albumin is not filtered across the glomerular capillary and would increase the oncotic pressure gradient, resulting in a lower net filtration pressure.
(Choice B) Alpha-1 receptors are located mainly in the afferent arteriole; alpha agonists (eg, epinephrine, norepinephrine) result in constriction of the afferent arteriole, which reduces hydrostatic pressure and leads to lower net filtration pressures.
(Choice D) Prostaglandins (eg, prostaglandin E2) are responsible for dilation of the afferent arteriole. Inhibition of prostaglandin synthesis, as seen with nonsteroidal anti-inflammatory drugs, results in constriction of the afferent arteriole, leading to reduced hydrostatic pressure and a lower net filtration pressure.
(Choice E) Vasopressin 2 antagonists (eg, tolvaptan) reduce vasopressin-induced free water resorption. These drugs do not have a direct effect on the Starling forces; however, reduced free water resorption can result in decreased blood volume, which decreases capillary hydrostatic pressure, which would lower the net filtration pressure.
Educational objective:
The net filtration pressure is a result of pressure gradients formed by Starling forces and is calculated by subtracting the oncotic pressure gradient from the hydrostatic pressure gradient. Angiotensin II preferentially constricts the efferent arteriole, resulting in an increased hydrostatic pressure gradient and an increased net filtration pressure.
A 69-year-old man is evaluated shortly after undergoing elective surgical repair of a descending thoracic aortic aneurysm. He has weakness in both lower extremities and urinary retention, which were not present before the procedure. The surgery was complicated by significant blood loss requiring multiple transfusions. The patient has a history of osteoarthritis, hypertension, hyperlipidemia, type 2 diabetes mellitus, and coronary artery disease. He also has 70% stenosis of his right carotid artery. Neurologic examination shows flaccid paralysis and loss of pain sensation in the lower extremities; vibratory sensation is intact. Upper extremity examination reveals no abnormalities. Which of the following is the most likely cause of this patient’s neurologic dysfunction?
- Cervical spondylotic myelopathy
- Epidural hematoma compressing the spinal cord
- Intraoperative cortical stroke
- Lumbar plexopathy
- Spinal cord infarction
Explanation:
Spinal cord (SC) ischemia is a devastating but not uncommon (~5%-15%) complication of thoracic aortic aneurysm (TAA) repair. TAA repair can disrupt SC blood flow: Aortic cross-clamping causes temporary SC hypoperfusion, and vascular graft placement (to recreate the luminal wall) can disrupt segmental arteries arising from the aorta. Because the anterior spinal artery relies on blood supply from these segmental arteries, the SC territory that it supplies—the anterior two-thirds of the SC—is particularly susceptible to ischemic infarct.
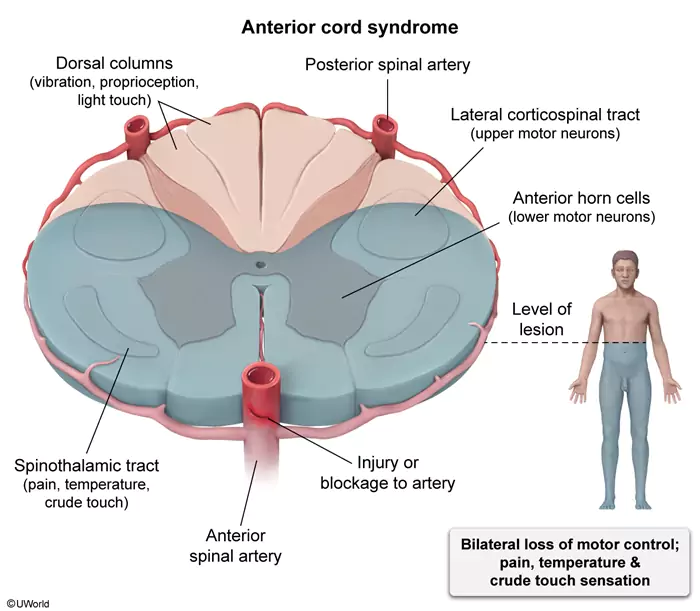
Infarction of the anterior SC results in anterior cord syndrome, with the following findings distal to the lesion:
- Bilateral paralysis from damage to the lateral corticospinal tracts and anterior horn cells
- Loss of pain/temperature and crude touch sensation from damage to the lateral and anterior spinothalamic tracts
- Urinary retention from damage to the descending autonomic tracts involved in bladder control
In contrast, the posterior spinal arteries, which arise off the vertebral/posterior inferior cerebellar artery, are intact and maintain perfusion to the posterior SC. Therefore, vibratory, proprioceptive, and light touch sensation (conveyed by the dorsal columns) are typically preserved.
Although flaccid paralysis due to spinal shock (ie, temporary loss of all distal SC function) occurs initially, upper motor neuron signs such as spasticity and hyperreflexia subsequently develop over days to weeks.
(Choice A) Neck hyperextension (eg, during intubation) in the setting of cervical spondylosis (ie, degenerative changes in the spine) classically causes central cord syndrome, characterized by disproportionately greater motor impairment in the upper extremities compared with the lower extremities.
(Choice B) SC compression from a spinal epidural hematoma can cause lower extremity motor and sensory deficits. However, epidural hematomas more commonly complicate procedures involving puncture of the spinal dura and are not a common complication of TAA repair.
(Choice C) Intraoperative hypoperfusion in the setting of right carotid artery atherosclerosis can cause a cortical stroke. However, this typically presents with unilateral, contralateral neurologic deficits rather than bilateral deficits.
(Choice D) Lumbar plexopathy, a peripheral neuropathy involving multiple adjacent nerve roots, can cause lower extremity weakness and diminished sensation. However, findings are typically asymmetric and focal (eg, unilateral footdrop) rather than symmetric and diffuse (eg, bilateral flaccid paralysis), and both pain/temperature and vibratory/proprioceptive sensation are affected.
Educational objective:
Thoracic aortic aneurysm repair can cause spinal cord ischemia, especially of the anterior cord. Anterior cord syndrome typically presents with distal, bilateral flaccid paralysis; loss of pain/temperature and crude touch sensation; and urinary retention.
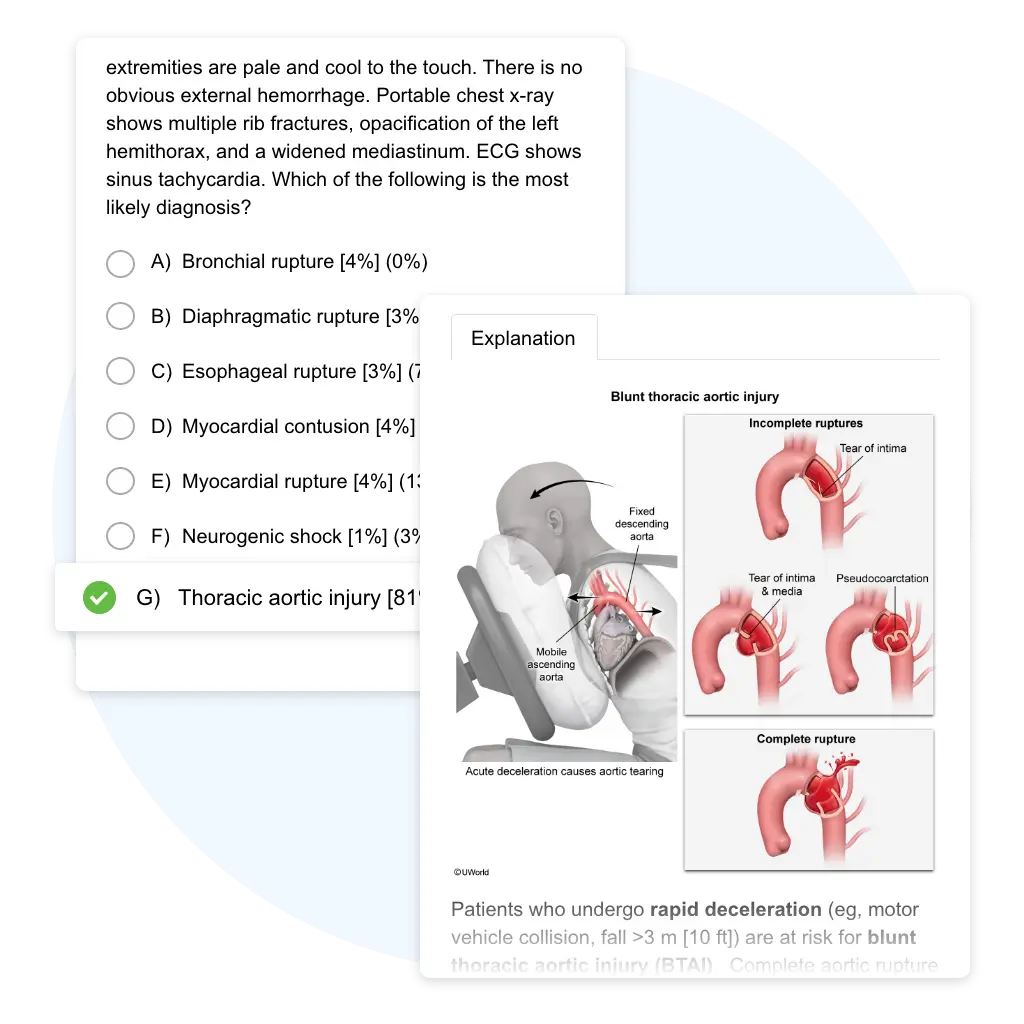
A 44-year-old man is brought to the emergency department after he was found unresponsive at the scene of a high-speed motor vehicle collision. The paramedics report that he was the unrestrained driver, and the passenger in his car was pronounced dead at the scene. The patient was intubated and rushed to the hospital. On arrival, his blood pressure is 78/40 mm Hg, pulse is 135/min, and pulse oximetry is 96% on mechanical ventilation with 40% oxygen. Rapid infusion of isotonic fluids is initiated. Trauma primary survey reveals an intubated man with appropriate spinal precautions. There is bruising and the imprint of the steering wheel across the anterior chest. The trachea is midline, and breath sounds are clear on the right but diminished on the left. Neck veins are collapsed bilaterally. Heart sounds are normal. All four extremities are pale and cool to the touch. There is no obvious external hemorrhage. Portable chest x-ray shows multiple rib fractures, opacification of the left hemithorax, and a widened mediastinum. ECG shows sinus tachycardia. Which of the following is the most likely diagnosis?
- Bronchial rupture
- Diaphragmatic rupture
- Esophageal rupture
- Myocardial contusion
- Myocardial rupture
- Neurogenic shock
- Thoracic aortic injury
Explanation:
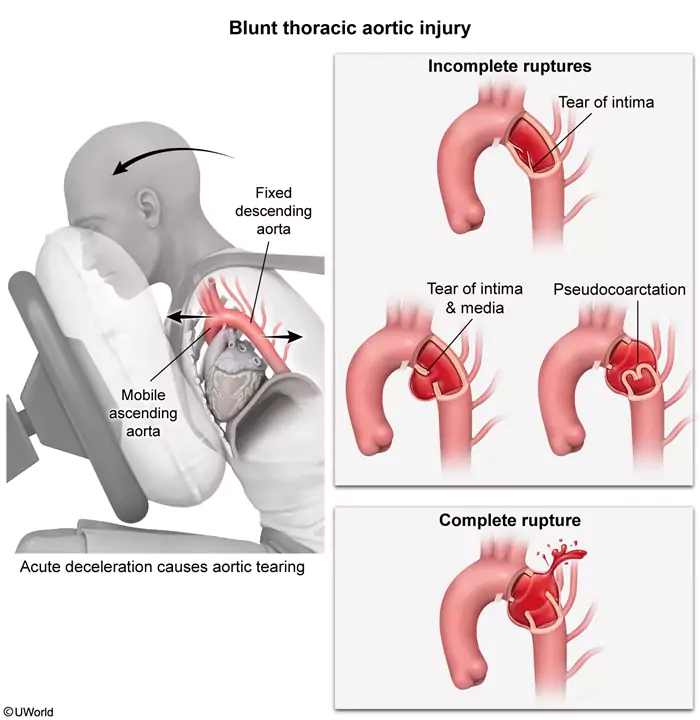
Patients who undergo rapid deceleration (eg, motor vehicle collision, fall >3 m [10 ft]) are at risk for blunt thoracic aortic injury (BTAI). Complete aortic rupture (ie, full-thickness tearing through intimal, medial, and adventitial layers) typically results in rapid exsanguination and death prior to hospital arrival. However, incomplete rupture (ie, adventitia still intact) may allow patients to survive long enough to receive medical attention. Likewise, patients with a complete rupture contained by a hematoma or surrounding tissues (as likely occurred in this patient) may survive the initial injury but require expedient evaluation and management to prevent rebleeding. They will likely be in hemorrhagic shock (hypotension, collapsed neck veins, pale and cool extremities).
Although external signs of blunt chest trauma (eg, bruising, steering wheel imprint) are concerning for BTAI, there are no clinical findings specific for aortic injury. Chest x-ray findings suggestive of BTAI include a widened mediastinum, abnormal (eg, enlarged) aortic contour, and/or left-sided effusion due to hemothorax (which explains this patient’s diminished breath sounds on the left). Concomitant injuries (eg, rib fractures) may be present. Diagnosis of BTAI can be confirmed via CT angiography for hemodynamically stable patients or transesophageal echocardiography (likely in the operating room) for unstable patients. Although hemodynamic support (eg, fluids, blood products) is indicated in hypotensive patients, systolic blood pressure is generally kept at <100 mm Hg to prevent injury extension and rebleeding while awaiting emergent operative repair.
(Choices A and B) Bronchial rupture causes rapid air leakage from the tracheobronchial tree, manifesting on chest x-ray as pneumothorax, pneumomediastinum, and/or subcutaneous emphysema. Diaphragmatic rupture presents on chest x-ray with loss of diaphragmatic contour and/or presence of abdominal organs within the thoracic cavity.
(Choice C) Chest x-ray findings of esophageal rupture may include widened mediastinum and pleural effusion (from accumulation of leaked esophageal contents). However, sudden-onset shock shortly after the insult makes BTAI much more likely. Mediastinitis from untreated esophageal rupture can result in septic shock but typically develops over hours to days (rather than minutes).
(Choice D) Myocardial contusion can cause hypotension and tachycardia but is classically accompanied by arrhythmia or new bundle branch block.
(Choice E) Myocardial rupture usually results in immediate death. Cardiac tamponade may result if the rupture is contained by the pericardium but would cause muffled heart sounds and distended neck veins.
(Choice F) Motor vehicle collisions may cause traumatic spinal cord injury. Associated disruption of the sympathetic nervous system can lead to neurogenic shock and hypotension; however, bradycardia would be expected rather than tachycardia.
Educational objective:
Rapid deceleration can cause blunt thoracic aortic injury (BTAI). Widened mediastinum on chest x-ray should increase suspicion for BTAI and left-sided pleural effusion (hemothorax) may be present from hemorrhage preceding containment (eg, hematoma). Strict blood pressure control and emergent surgical intervention are necessary to prevent rebleeding and death.
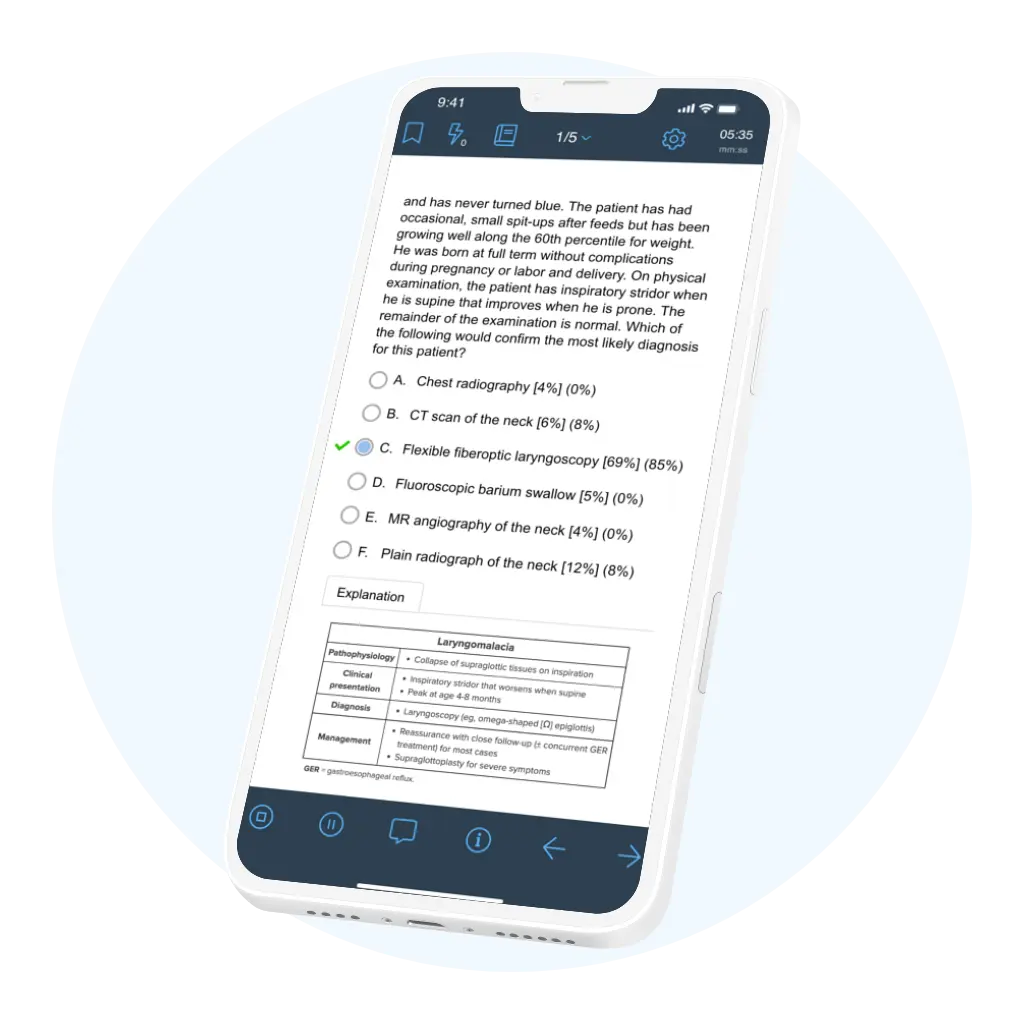
A 4-month-old boy is brought to the office for “noisy breathing.” The patient’s parents first noticed a harsh sound when he cried at age 2 weeks, but it has gotten louder over the past month, especially when he is lying on his back. The noise seems to improve when the patient is held upright or during “tummy time.” He does not appear to have labored breathing and has never turned blue. The patient has had occasional, small spit-ups after feeds but has been growing well along the 60th percentile for weight. He was born at full term without complications during pregnancy or labor and delivery. On physical examination, the patient has inspiratory stridor when he is supine that improves when he is prone. The remainder of the examination is normal. Which of the following would confirm the most likely diagnosis for this patient?
- Chest radiography
- CT scan of the neck
- Flexible fiberoptic laryngoscopy
- Fluoroscopic barium swallow
- MR angiography of the neck
- Plain radiograph of the neck
Explanation:
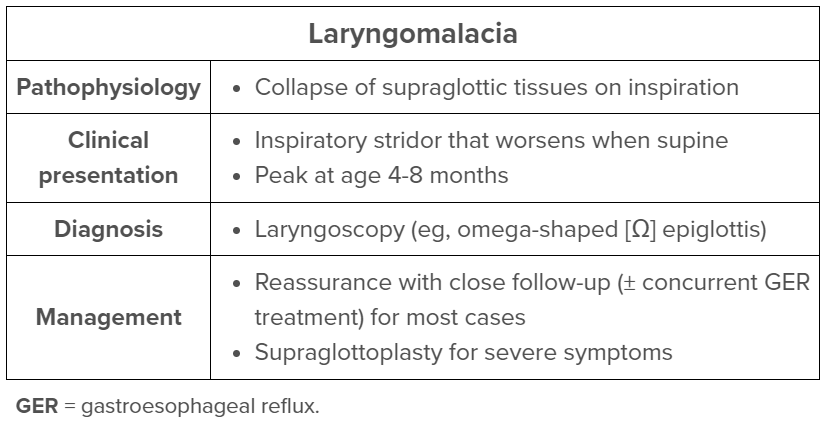
Laryngomalacia, which causes chronic stridor in infants, is typified by “floppy” supraglottic structures that collapse during inspiration. Proposed pathophysiologic etiologies include laryngeal hypotonia (due to delayed maturation or neuromuscular disorder), redundant supraglottic soft tissue, and inflammation (due to reflux).
Stridor from laryngomalacia usually begins in the neonatal period and is loudest at age 4-8 months. Presentation includes inspiratory stridor that is worse in the supine position and exacerbated by feeding or upper respiratory illnesses; prone positioning improves symptoms. The diagnosis is confirmed with visualization of the larynx, typically by flexible fiberoptic laryngoscopy. Findings include an omega-shaped (Ω) epiglottis and collapse of the supraglottic structures during inspiration.
Gastroesophageal reflux (GER) treatment often improves symptoms; it is unclear whether GER causes laryngomalacia or is due to a common underlying mechanism (eg, neuromuscular disorder). Most infants with laryngomalacia will feed, grow, and ventilate normally with spontaneous resolution of stridor by age 18 months. Infants with feeding difficulties, tachypnea, cyanosis, or failure to thrive may require surgery to remove redundant supraglottic tissues.
(Choice A) Chest radiographs can identify anterior mediastinal masses and radiopaque foreign bodies, both of which can cause stridor. Mediastinal masses (eg, lymphoma) also present with systemic symptoms (eg, fever, weight loss, lymphadenopathy), and airway foreign bodies present with a more acute symptom onset; these symptoms are not seen in this patient.
(Choices B and F) Retropharyngeal abscesses occur in toddlers and present with fever, dysphagia, neck pain, and stridor. Lateral neck radiographs can demonstrate thickening of the prevertebral space. CT scan of the neck can better define extension of the abscess to nearby structures. This patient does not have symptoms suggestive of infection.
(Choices D and E) Vascular rings occur when an anomalous branch of the aortic arch or pulmonary artery encircles the trachea and esophagus. They may cause biphasic or expiratory stridor due to tracheal compression and feeding difficulties due to esophageal compression. A barium swallow can identify indentations of the esophagus, and the diagnosis can be confirmed with contrasted CT scan or MR angiography.
Educational objective:
Laryngomalacia presents in infants with inspiratory stridor that worsens in the supine position and improves in the prone position. Laryngoscopy shows collapse of the supraglottic structures during inspiration. Concurrent gastroesophageal reflux should be treated. Laryngomalacia usually resolves spontaneously by age 18 months.
A bedside ultrasound reveals a low, posterior placenta that extends over the internal cervical os. The patient continues to have heavy vaginal bleeding, and a cesarean delivery is performed under spinal anesthesia. The neonate and placenta are delivered without difficulty. During repair of the uterine incision, she reports difficulty breathing shortly before becoming unresponsive. Blood pressure is 70/40 mm Hg, pulse is 124/min, and respirations are 34/min. Pulse oximetry is 86% on room air. A lung examination reveals decreased breath sounds bilaterally. Endotracheal intubation is performed, and the airway is secured. Profuse bleeding is noted from the uterine incision and placental bed. Examination of the Foley catheter reveals frank blood in the collection bag. Which of the following most likely led to this patient’s decompensation?
- Amniotic fluid embolism
- High spinal anesthesia
- Local anesthetic systemic toxicity
- Placenta accreta
- Preeclampsia with pulmonary edema
Explanation:
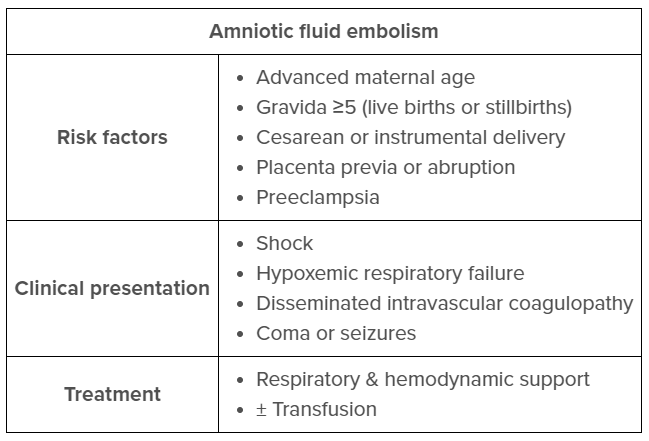
This patient has acute-onset hypoxemia, hypotension, and disseminated intravascular coagulopathy (eg, hematuria, hemorrhage), a presentation consistent with amniotic fluid embolism syndrome (AFES).
AFES, a rare but catastrophic complication of pregnancy, typically occurs during labor or in the immediate postpartum period. Amniotic fluid enters the maternal circulation through the endocervical veins, the placental implantation site, or areas of uterine trauma (eg, cesarean incision site). The amniotic fluid triggers a massive anaphylactoid reaction that results in vasospasm, obstructive shock, pulmonary edema, respiratory failure, seizures, and disseminated intravascular coagulation.
Risk factors for AFES include cesarean/operative delivery, placenta previa, and abruptio placentae. Treatment is supportive, focusing on correcting hypoxemia (eg, oxygen, intubation), hypotension (eg, vasopressors, transfusion), and blood loss (eg, massive transfusion protocol). AFES is associated with a high risk of maternal and neonatal mortality and, among survivors, a high risk of significant neurologic sequelae.
(Choice B) High spinal anesthesia occurs when the local anesthetic agent used in neuraxial anesthesia spreads to a more cephalad spinal level than intended. High spinal anesthesia typically presents with hypotension due to loss of sympathetic response and dyspnea due to paralysis of the diaphragm and other respiratory muscles. There is no associated coagulopathy, making the diagnosis unlikely in this patient.
(Choice C) Local anesthetic toxicity can rarely occur with epidural analgesia (eg, bupivacaine). When the anesthetic is absorbed into the maternal circulation, it initially blocks inhibitory neural pathways to cause CNS overactivity (eg, perioral numbness, tinnitus), potentially followed by seizure. Patients often develop increased cardiovascular sympathetic activity (eg, hypertension, tachycardia), followed by cardiovascular collapse.
(Choice D) Placenta accreta, the direct attachment of the placenta to the myometrium, can present with difficulty separating the placenta from the uterus after fetal delivery and with a postpartum hemorrhage that can lead to coagulopathy. This diagnosis is unlikely because the placenta was delivered without difficulty.
(Choice E) Preeclampsia can present with complications of pulmonary edema and coagulopathy; however, the diagnosis requires hypertension, which is not seen in this patient.
Educational objective:
Amniotic fluid embolism syndrome (AFES) presents during labor or immediately postpartum with acute onset of hypoxemia, hypotension, and disseminated intravascular coagulopathy. AFES is a massive inflammatory response due to the release of fetal amniotic fluid into the maternal circulation. Treatment is supportive.
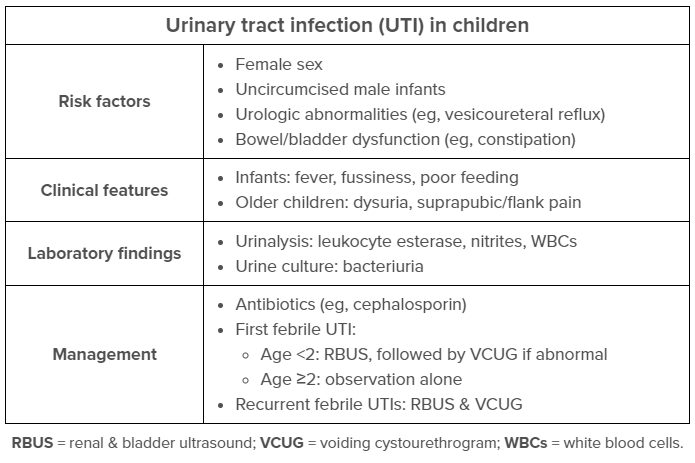
A 6-month-old boy is brought to the office by his mother due to fever for 3 days. He has been irritable for the past 2 days. The patient normally drinks 6-oz bottles of expressed breast milk, but he has been taking < 3 oz per feed and voiding less frequently than usual. He has had no rash, cough, congestion, vomiting, or diarrhea. The patient takes no medications and has no known allergies. Temperature is 38.9 C (102 F). He is irritable but easily consoled by his mother. Mucous membranes are moist, and tears are present with crying. Tympanic membranes are gray and translucent bilaterally, and the oropharynx is normal. Cardiopulmonary examination is normal. The abdomen is soft, nontender, and nondistended. The penis is uncircumcised. Urine catheterization is performed, and urine dipstick analysis reveals the following:
| Specific gravity | 1.020 |
| Protein | none |
| Blood | trace |
| Leukocyte esterase | moderate |
| Nitrites | positive |
Oral antibiotics are started, and the patient is afebrile within 36 hours. Urine culture yields >50,000 colony-forming units of Escherichia coli. After completion of the therapeutic antibiotic course, which of the following is the best next step in management of this patient?
- Begin prophylactic antibiotics
- No other intervention is indicated
- Perform renal and bladder ultrasound
- Perform renal scintigraphy
- Recommend circumcision
Explanation:
This patient has a urinary tract infection (UTI), which is defined by the presence of pyuria (leukocyte esterase on dipstick analysis, white blood cell count of >5/hpf on microscopy) and bacteriuria. Although classic symptoms in older children include dysuria or abdominal pain, a high degree of suspicion must be maintained in infants because clinical features are often nonspecific (eg, fever, poor feeding, irritability). Risk factors include lack of circumcision in infant boys and genitourinary abnormalities (eg, vesicoureteral reflux [VUR]).
All children age <2 with a febrile UTI should undergo renal and bladder ultrasound (RBUS) to evaluate for hydronephrosis and ureteral dilation, which may suggest an underlying anatomic abnormality (eg, VUR). RBUS can be delayed until a second febrile UTI in children age ≥2 due to a lower risk for anatomic abnormalities, which usually cause complications at an earlier age (Choice B). Ultrasound should be performed after the acute illness has been treated (ie, antibiotic course) because renal inflammation during the acute infection can lead to false-positive results.
A normal ultrasound makes the likelihood of underlying VUR low, and no further imaging or management (eg, prophylactic antibiotics) is required (Choice A). Patients with an abnormal RBUS or recurrent febrile UTIs, however, should undergo a voiding cystourethrogram to identify potential VUR, which often requires treatment with prophylactic antibiotics.
(Choice D) Renal scintigraphy uses abnormalities in dimercaptosuccinic acid uptake to detect scarring (indicative of VUR) in the chronic setting. Unlike RBUS, it is an invasive test that exposes children to radiation and is therefore not recommended following a first UTI.
(Choice E) Uncircumcised boys have an increased risk for UTI during infancy compared with circumcised boys. However, overall rates of UTI are still very low, and identification of potential urinary tract defects with RBUS should be prioritized over consideration of an elective circumcision that is not medically necessary.
Educational objective:
After a first-time febrile urinary tract infection, children age <2 should undergo renal and bladder ultrasound to evaluate for anatomic abnormalities (eg, vesicoureteral reflux). Those with recurrent infections or abnormal ultrasound findings should also undergo a voiding cystourethrogram.
A 7-year-old boy is brought to the emergency department due to a dog bite to the face. The father states the patient approached their dog, who was sleeping, and the dog suddenly snapped and bit him near the right eye. The dog’s vaccines are up to date. The patient has no medical conditions, and his vaccines are up to date. Vital signs are normal. On examination, there are 2 puncture wounds on the lateral forehead. The right eyelid is swollen, and there is a small, horizontal laceration of the lateral aspect of the right upper eyelid; there is fatty tissue protruding at the base of the wound. The pupils are symmetric and reactive to light, and the extraocular movements are intact. Visual acuity is normal. Which of the following structures is most likely injured as a result of the eyelid laceration in this patient?
- Canaliculi
- Levator muscle
- Nasolacrimal duct
- Nasolacrimal sac
- Punctum
Explanation:
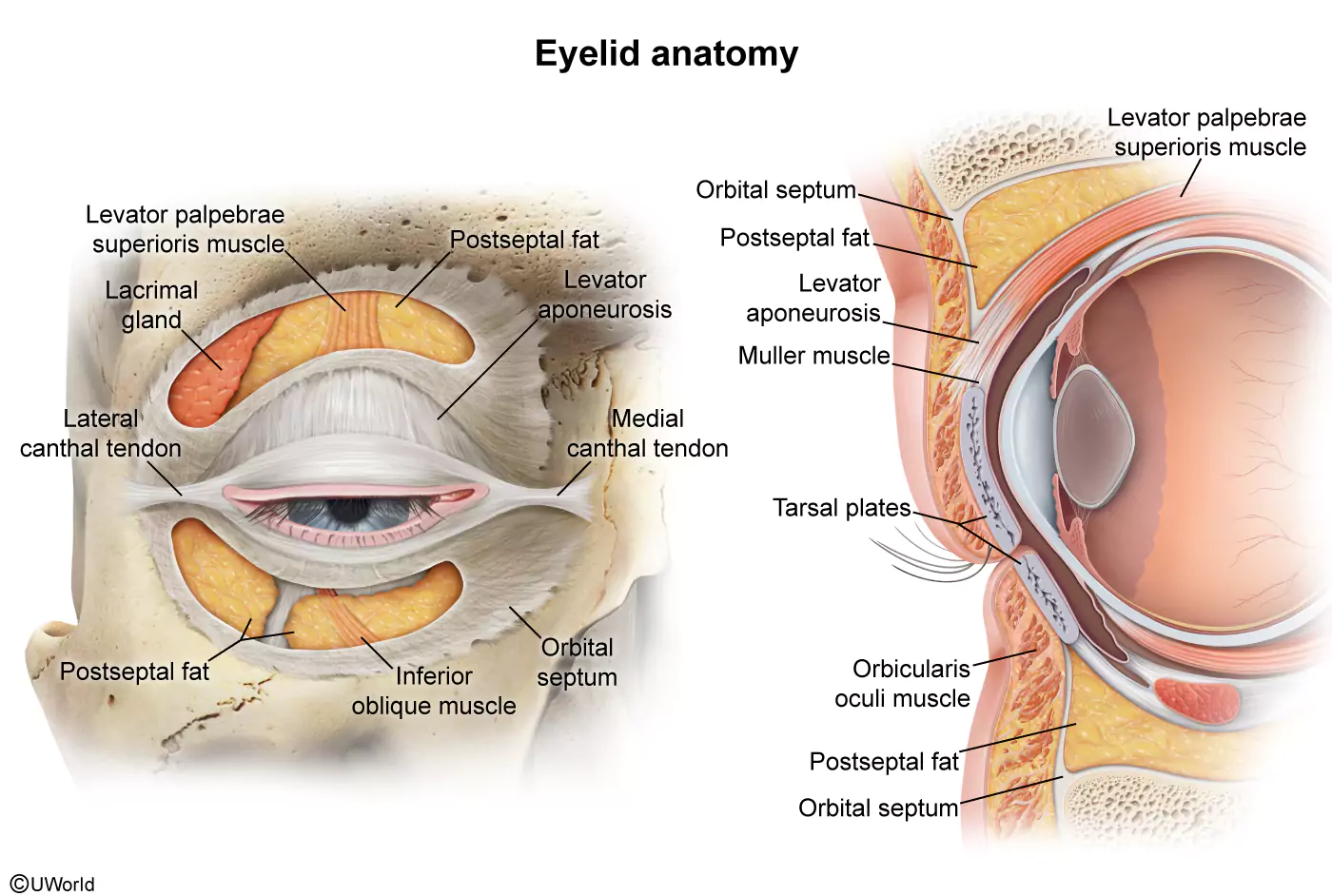
This patient with an upper eyelid laceration has fat protruding from the wound, which is consistent with injury to the orbital septum. The orbital septum is made of fibrous tissue and acts as a barrier between the preseptal and postseptal structures, which include the following:
- Preseptal: eyelid skin and orbicularis oculi muscle
- Postseptal: orbital fat, eyelid retractors (eg, levator palpebrae superioris muscle and aponeurosis), and extraocular muscles (eg, superior rectus muscle)
The (postseptal) orbital fat lies just behind the orbital septum and protects the deeper structures. Therefore, visible or protruding fat at the base of a wound (eg, upper eyelid laceration) indicates that the septum has been violated and that the deeper structures such as the levator muscle may be injured as well. In patients with upper eyelid laceration, eyelid drooping or decreased voluntary eyelid retraction would also suggest levator muscle injury, although eyelid swelling can make these signs more difficult to observe.
Prior to repair of this laceration, CT scan should be obtained to assess the extent of damage and rule out globe injury. Complex eyelid lacerations such as this one should then be repaired by a qualified surgeon in the operating room.
(Choices A, C, D, and E) Eyelid lacerations can involve the punctum, canaliculi, nasolacrimal duct, or nasolacrimal sac; however, these structures are most susceptible to injury with medial eyelid lacerations. In contrast, the lacrimal gland, a postseptal structure located near the orbital rim, may be injured with lateral upper eyelid lacerations. If not repaired appropriately, lacerations involving the nasolacrimal system can result in permanent tearing.
Educational objective:
The orbital septum separates preseptal structures (ie, eyelid skin and orbicularis oculi muscle) from postseptal structures (ie, orbital fat, eyelid retractors, extraocular muscles). In an eyelid laceration, visible fat within the wound is consistent with orbital septal injury and raises concern for injury to other postseptal structures such as the levator muscle.
Relevant USMLE Questions & Cases
Every question and case in your USMLE QBank is designed with your future clinical success in mind. From high-yield Step 1 MCQs to interactive Step 3 CCS cases, our content mirrors your exam while keeping pace with the latest medical standards—so your study time always counts.
In our Step 2 CK QBank, you’ll even find shelf exam questions seamlessly integrated and presorted. That means you can prepare for rotations and Step 2 simultaneously, saving time and maximizing your efficiency as you build exam-ready confidence.
USMLE QBank Success Stories
UWorld USMLE Product Tour
Frequently Asked Questions
Yes, each UWorld Medical QBank adheres to the equivalent NBME content outline. By completing your QBank, you will have reviewed the clinical content required to pass your exam.
Yes, all UWorld Medical questions are written in the style of your exam. For example, Step 3 contains Computer-based Case Simulations (CCS cases), which we provide to help you prepare.
Our team of physicians recommends doing as many questions as you can reasonably accomplish early on (get acclimated with about 30 minutes per day), building up to 10-20 questions per day. The key is to take in the information and not overload yourself. The goal should be to complete two full passes of your QBank, once before dedicated study and once during it.