Free AKT Exam Sample Questions
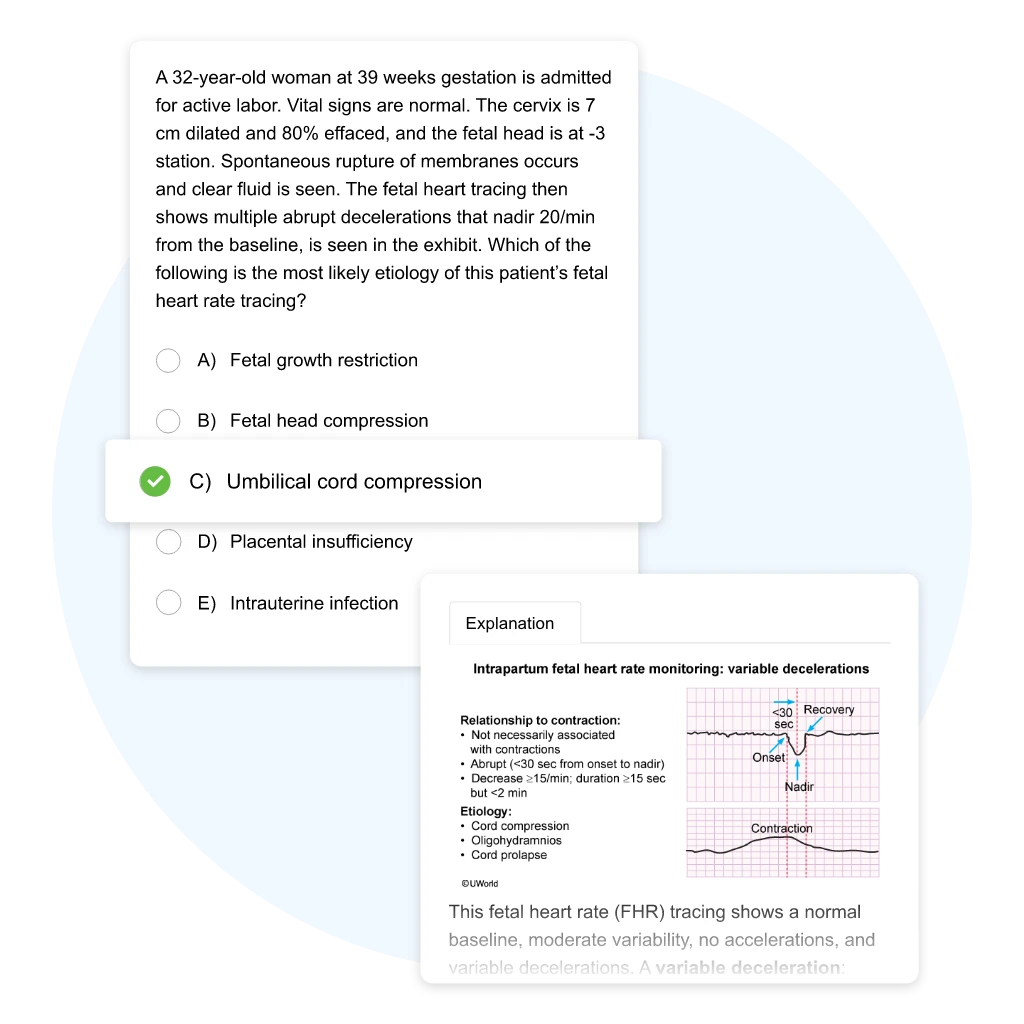
Practising with exam-like questions is an essential part of preparing for the AKT section of the UKMLA exam. Try these free UWorld AKT questions to see how our in-depth explanations and award-winning illustrations help students understand difficult clinical concepts on a deeper level.
Benefits of Practising AKT-Style Questions
UWorld AKT questions and explanations are written by practising doctors to cover the medical concepts you need to know to be successful in the classroom and on the exam.
Benefit from Active
and Visual Learning
Customise Quizzes to
Fit Your Needs
Learn from Premier
Answer Explanations
Free AKT Questions - See the UWorld Difference
UWorld AKT questions reflect the latest UKMLA MCQ format and structure to ensure that you're prepared for exam day. See what you can expect from our question bank by trying a few sample questions and reading our award-winning explanations.
A 69-year-old man comes in due to progressive bilateral loss of vision over the past several months. The patient has issues with his central vision, but his peripheral field and navigational vision are not affected. Two years ago, he had cataracts removed from both eyes. Which of the following is the most likely diagnosis?
| A. Central retinal artery occlusion | ||
| B. Macular degeneration | ||
| C. Open-angle glaucoma | ||
| D. Recurrent cataracts | ||
| E. Retinal detachment |
Explanation:
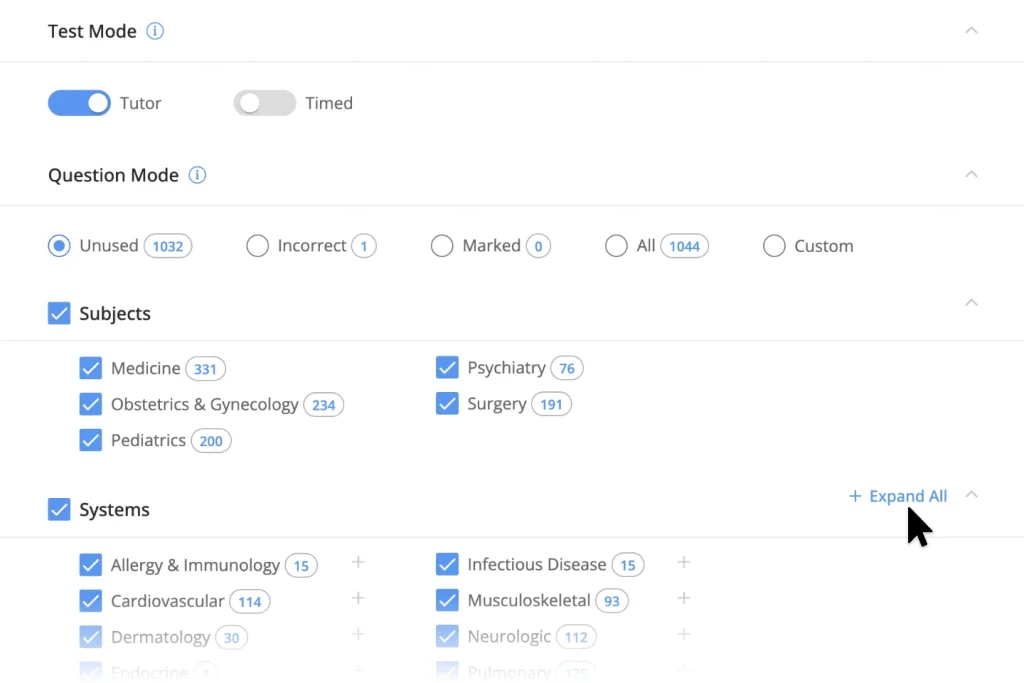
This patient with progressive, painless vision loss has age-related macular degeneration (AMD), which is a major cause of blindness and visual impairment in older adults (age >50). AMD occurs due to the progressive degeneration of the retinal epithelium, typically due to increasing age. Early findings in AMD include the distortion and wavy appearance of straight lines on the Amsler grid test. As the disease progresses, patients develop progressive and bilateral loss of central vision. Peripheral fields and navigational vision (allowing patients to navigate around obstacles in their surroundings and maintain social independence) are classically maintained, although they may become impaired due to the development of cataracts. On physical examination, patients with advanced disease often have characteristic drusen deposits in the macula.
(Choice A) Central retinal artery occlusion is a condition with sudden onset of complete monoocular vision loss due to acute retinal ischemia due to thrombosis or emboli in the central retinal artery (branch of ophthalmic artery).
(Choice C) Open-angle glaucoma usually presents as a gradual loss of peripheral vision (over a period of years) and consequent tunnel vision. Central vision is spared.
(Choice D) Once removed, cataracts do not typically recur. Following cataract surgery, some patients develop posterior capsule opacification (thickening of the capsule holding the artificial lens), which can cause cloudy vision and can be treated (eg, with laser) without resulting in long-term vision problems. Progressive central vision loss with maintenance of peripheral vision is highly suggestive of AMD.
(Choice E) Retinal detachment presents with a sudden onset of flashes of light, floaters, and painless vision loss (peripheral followed by central). It is usually associated with severe myopia, aging, trauma, or previous eye surgery.
Educational objective:
Age-related macular degeneration is usually seen in patients age >50. It presents with progressive and bilateral loss of central vision. Navigational vision is preserved.
A 63-year-old man presents with sharp, stabbing pain on the right side of the face and hiccups that started 6 hours ago. The patient is right-handed and has been unable to feed himself since his symptoms started. He has a history of stable angina, hypertension, and hyperlipidemia. Vital signs are normal. The patient has horizontal and vertical nystagmus and ptosis of the right eye. Gag reflex is diminished. He reports loss of pain and temperature sensation on the right side of the face and left trunk and limbs, as well as severe dizziness when attempting to stand. Which of the following is the most likely location of this patient's brain lesion?
| A. Lateral cerebellar hemisphere | ||
| B. Lateral medulla | ||
| C. Lateral mid-pons | ||
| D. Medial medulla | ||
| E. Medial mid-pons |
Explanation:
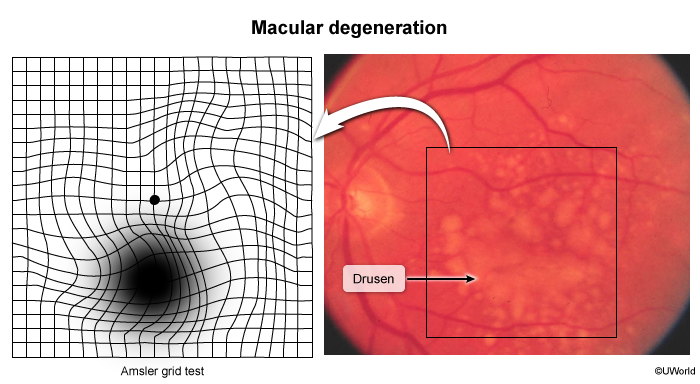
This patient has had a stroke that resulted in lower cranial nerve nuclei deficits (eg, vertigo, decreased gag) and loss of pain and temperature sensation of the right face (trigeminal nucleus) and left body (spinothalamic tract). Because the brainstem is where most cranial nerves originate and many motor and sensory fibers cross the midline, brainstem strokes characteristically lead to ipsilateral cranial nerve deficits and contralateral deficits of the body (ie, crossed signs). In addition, this patient has the following:
- Vertigo and nystagmus, suggesting a vestibulocochlear nerve (CN VIII) deficit, and bulbar weakness (eg, weak gag, dysphagia), suggesting glossopharyngeal nerve (CN IX) and/or vagus nerve (CN X) dysfunction. Each of these cranial nerves has nuclei in the lateral medulla (vestibular nucleus, nucleus ambiguus).
- Loss of pain and temperature sensation in the ipsilateral face and contralateral body due to damage to the spinal trigeminal nucleus and spinothalamic tract
- Ipsilateral Horner syndrome due to damage of descending sympathetic nervous system fibers that travel near the spinothalamic tract
This constellation of findings is consistent with lateral medullary (Wallenberg) syndrome. Because the corticospinal tract travels medially in the entire brainstem before crossing at the lower medulla, most lateral brainstem lesions do not have dense contralateral hemiplegia.
(Choice A) Although lesions of the lateral cerebellar hemisphere present with dizziness and ipsilateral ataxia, they do not cause Horner syndrome or loss of pain and temperature sensation.
(Choices C and E) Pontine lesions can also lead to ataxia due to disruption of the cerebellar peduncles and vestibular nuclei. However, this patient's dysphagia, hoarseness, and diminished gag reflex are due to CN IX and/or CN X involvement, suggesting damage to the nucleus ambiguus, located in the medulla. The nuclei for cranial nerves V-VIII originate in the pons.
(Choice D) Unlike the lateral medulla, which contains many tracts, the medial medulla mainly contains the hypoglossal nerve (CN XII) and the corticospinal tract. Patients with medial medullary syndrome develop contralateral hemiparalysis and ipsilateral CN XII palsy (tongue deviation toward the lesion).
Educational objective:
A lateral medullary infarct (Wallenberg syndrome) leads to vertigo/nystagmus (vestibular nucleus), loss of pain/temperature sensation in the ipsilateral face (trigeminal) and contralateral body (spinothalamic), bulbar weakness (lower cranial nerves), and ipsilateral Horner syndrome (descending sympathetic).
A 65-year-old man comes is evaluated due to an unsteady gait and frequent falls over the past 2 months. His left side feels "weak," which makes it difficult to maintain balance when walking or standing. He has also had headaches and nausea, which often awaken him from sleep. Vital signs are normal. Ambulation results in the patient swaying to the left and using the wall to brace himself. There is increased resistance to passive flexion of the left upper and lower extremity. Which of the following is the most likely cause of his current condition?
| A. Brain tumor | ||
| B. Hemiplegic migraine | ||
| C. Normal-pressure hydrocephalus | ||
| D. Parkinson disease | ||
| E. Vitamin B12 deficiency |
Explanation:
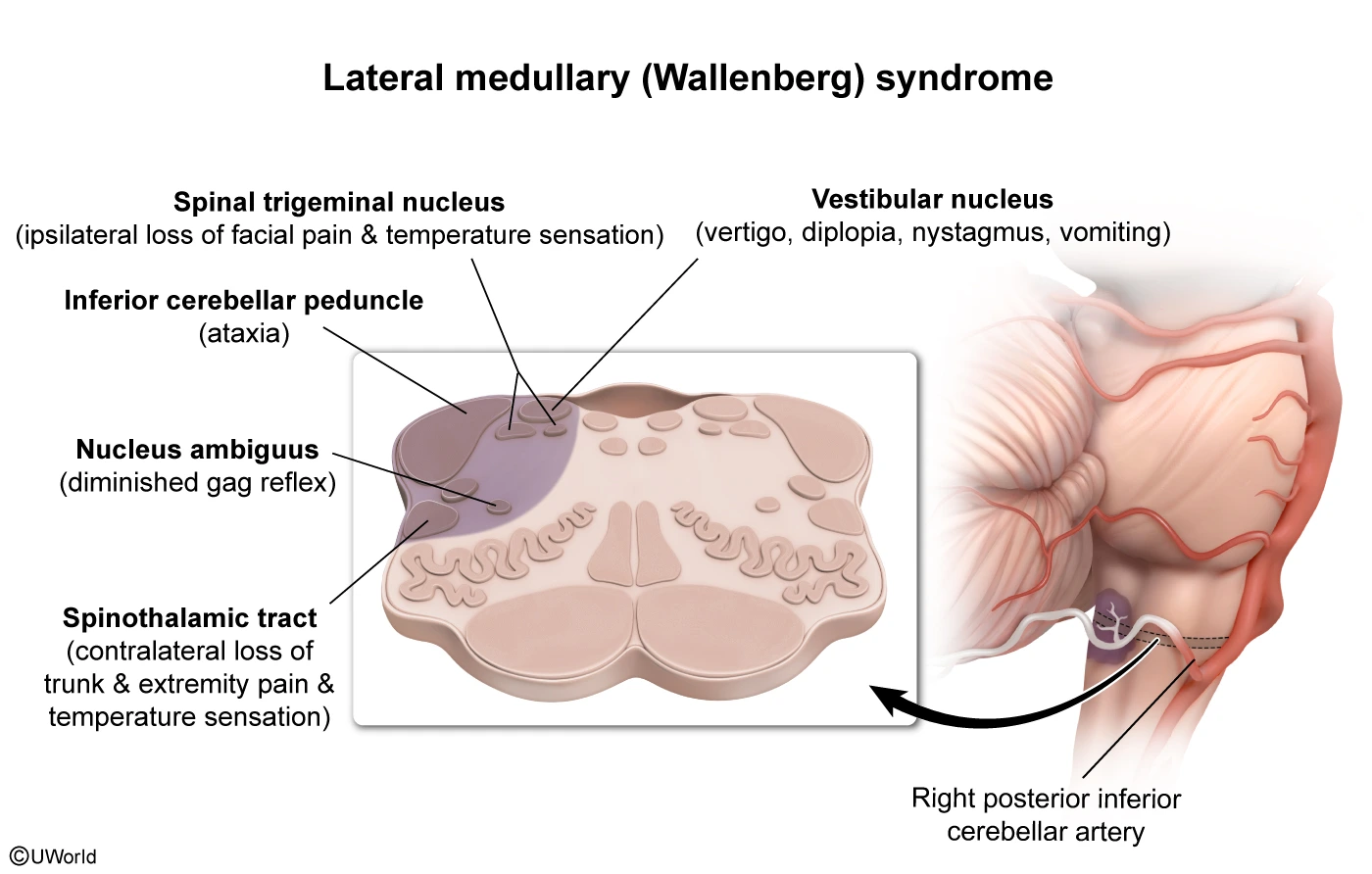
This patient has gait dysfunction, headaches with nausea that awaken him from sleep, and focal left-sided weakness with spasticity, raising concern for an intracranial tumor affecting the motor cortex.
Brain tumors are often clinically silent until they grow large enough to compress neurologic structures or raise intracranial pressure (ICP). The most common symptom is a dull headache associated with ≥1 of the following:
- Nausea and vomiting (due to increased ICP)
- Focal neurologic manifestations (due to tumor invasion or compression)
- Symptoms worsening during the night or with positions that raise ICP (eg, bending, coughing)
Funduscopic examination showing papilledema, a sign of elevated ICP, supports the diagnosis. Patients usually require MRI of the brain for further evaluation.
(Choice B) A hemiplegic migraine usually causes a combination of neurologic findings and headache that last hours (not months) and resolve completely. Hemiplegic migraines are quite rare and typically occur in teenagers (not elderly patients).
(Choice C) Normal-pressure hydrocephalus is caused by impaired cerebrospinal fluid absorption and usually causes shuffling gait, cognitive decline, and urinary incontinence. Unilateral weakness is atypical.
(Choice D) Parkinson disease is a progressive neurodegenerative disorder characterized by resting tremor, rigidity, and shuffling gait. Focal weakness and a new headache are more indicative of a brain tumor.
(Choice E) Vitamin B12 deficiency typically presents with progressive symmetric paresthesias and sensory ataxia, not unilateral weakness.
Educational objective:
Patients with an intracranial mass often have headache associated with nausea and vomiting and/or focal neurologic deficits. Symptoms are often worse at night and with body positioning that increases intracranial pressure.
A 20-year-old man is evaluated due to fever, headache, and neck pain that have lasted a day. Temperature is 38.7 C (101.7 F), blood pressure is 120/72 mm Hg, pulse is 112/min, and respirations are 26/min. There is neck stiffness and a petechial rash on the trunk. Cerebrospinal fluid (CSF) analysis reveals the following:
| Glucose | 30 mg/dL (1.67 mmol/L) |
| Protein | 180 mg/dL (1.8 g/L) |
| Leukocytes | 1,500/mm3 (1.5 × 109/L) |
| Neutrophils | 70% (0.70) |
CSF gram stain shows gram-negative diplococci. Suddenly, the patient's hemodynamic status deteriorates rapidly. Blood pressure drops to 80/50 mm Hg, and venous access sites are oozing blood. Which of the following findings is most likely to be seen on this patient's peripheral smear?
| A. Eosinophilia | ||
| B. Howell-Jolly bodies | ||
| C. Hypersegmented neutrophils | ||
| D. Rouleaux formations | ||
| E. Schistocytes |
Explanation:
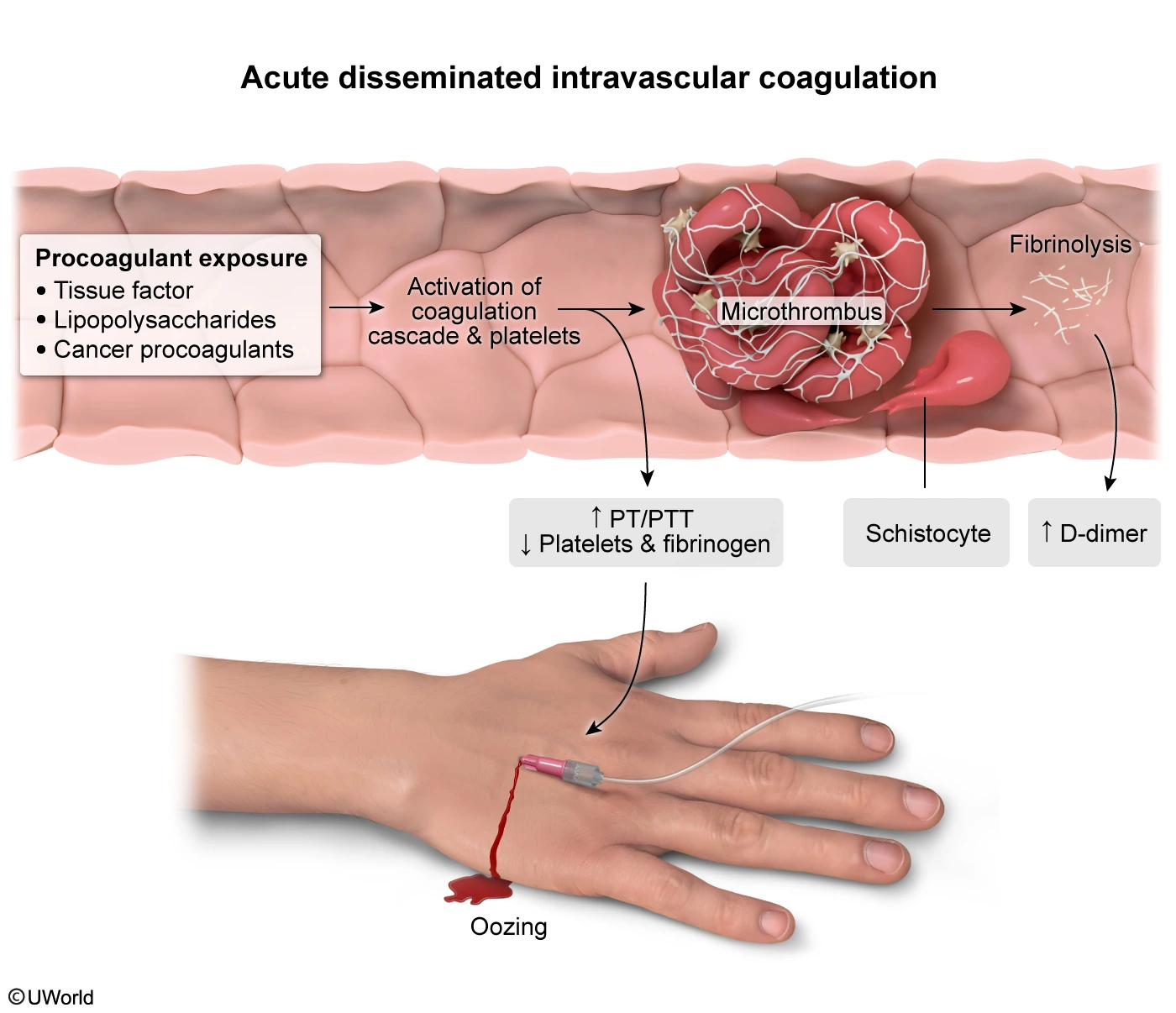
This patient's clinical findings (fever, headache, neck stiffness, rash) and cerebrospinal fluid analysis (elevated protein, low glucose, leukocytosis, gram-negative diplococci) are indicative of meningococcal meningitis; he subsequently developed septic shock (ie, severe hypotension) while in the emergency department. His bleeding from venous puncture sites highly suggests disseminated intravascular coagulation (DIC), a consumptive coagulopathy associated with sepsis, malignancy, trauma, and obstetric complications.
In DIC due to gram-negative sepsis, the coagulation cascade is activated by bacterial endotoxins, leading to widespread fibrin deposition and the consumption of coagulation factors and platelets that eventually results in bleeding. Deposition of fibrin strands in small vessels can cause shearing of circulating erythrocytes, resulting in schistocytes (fragmented erythrocytes) on peripheral smear. Laboratory values in DIC typically show decreased platelet count and fibrinogen levels and prolonged PT and PTT (indicating a consumption of coagulation factors).
(Choice A) Eosinophilia (ie, increased serum eosinophils) is typically associated with parasitic infections, allergies, and some malignancies. This patient with gram-negative diplococci on CSF analysis would have significant neutrophilia in response to a bacterial infection.
(Choice B) Howell-Jolly bodies are round, dark, purple/red inclusions within erythrocytes. These represent nuclear fragments that are typically removed by the spleen; they can be seen in patients with splenectomy or reduced splenic function (eg, sickle cell).
(Choice C) Hypersegmented neutrophils are characterized by nuclei with ≥5 lobes. They are a feature of megaloblastic anemia (vitamin B12 or folate deficiency).
(Choice D) Rouleaux formations are seen as stacked red blood cells on peripheral smear due to increased fibrinogen levels or other serum protein elevations (eg, multiple myeloma). Rouleaux formations are unlikely to develop in DIC due to decreased fibrinogen levels.
Educational objective:
Disseminated intravascular coagulation is a common complication of gram-negative bacterial sepsis due to activation of the coagulation cascade by bacterial endotoxins, which leads to the formation of microthrombi. Peripheral smear shows fragmented erythrocytes (schistocytes) and thrombocytopenia. Laboratory tests show decreased fibrinogen levels and prolonged PT and PTT.
A 68-year-old man with type 2 diabetes mellitus has had right knee pain for the last several months. The pain is exacerbated by activity and occasionally associated with transient swelling but no warmth or fever. The patient was also diagnosed with gout 5 years ago, and it is treated chronically with low-dose allopurinol. He drinks 1 or 2 beers a day. Vital signs are normal. BMI is 32 kg/m2. The right knee is not swollen or erythematous, but active range of motion elicits pain. Hemoglobin A1c is 7.3% and serum uric acid level is 5.2 mg/dL (normal: 3.0-8.2). Knee x-ray is shown in the exhibit. Which of the following interventions would provide the greatest long-term benefit for this patient's current symptoms?
| A. Acetaminophen therapy | ||
| B. Alcohol cessation | ||
| C. Improved glycemic control | ||
| D. Increased allopurinol dosage | ||
| E. Weight loss |
Explanation:
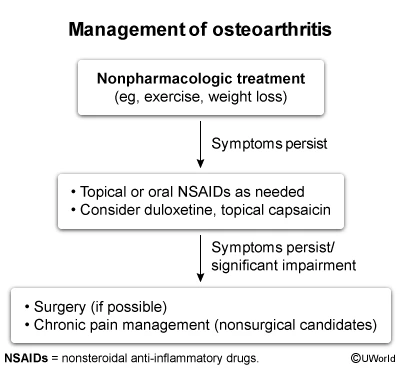
This patient has osteoarthritis (OA) of the knee with chronic joint pain that is worse with activity. The x-ray shows joint space narrowing at the patellofemoral compartment (bone on bone) with extensive osteophyte formation; knee OA classically affects the tibiofemoral joint, but the patellofemoral compartment may be involved as well. Risk factors for knee OA include age >40, obesity, abnormal joint alignment (eg, varus deformity), and prior joint injury.
Initial management of knee OA should include regular, low-impact aerobic activity (eg, walking, cycling) and weight loss, particularly in overweight and obese patients. Weight loss decreases the inflammation and joint loading that promote degeneration of the articular cartilage and is associated with decreased pain and functional impairment. There is a dose-response relationship between amount of weight lost and improvement in joint symptoms. Caloric restriction may contribute to loss of lean mass and therefore should be combined with muscle-strengthening exercises. Exercises to strengthen the quadriceps muscles can improve function and protect the articular cartilage from further stress.
(Choice A) The benefits of acetaminophen in osteoarthritis are small and inconsistent and likely do not outweigh the adverse effects (eg, hepatotoxicity) for most patients.
(Choice B) Alcohol intake is associated with the degradation of articular cartilage and worse OA symptoms. However, the effect of moderate alcohol use is relatively minor, and the benefits of an effective weight-loss program would have the greatest impact.
(Choice C) Chronic hyperglycemia can accelerate the progression of OA, likely due to glycosylation of components of articular cartilage. However, this patient's hemoglobin A1c is only slightly elevated, and stricter diabetes control would likely have little effect on his OA. In addition, in elderly (age >65) patients, a target hemoglobin A1c of 7%-8% is generally recommended to avoid dangerous hypoglycemia.
(Choice D) Allopurinol is used for prophylactic therapy in gout, which typically presents with acute attacks of redness, warmth, and swelling; it is not used for OA. In addition, this patient's uric acid level is <6 mg/dL, which is usually adequate to prevent gout attacks.
Educational objective:
Initial management of osteoarthritis of the knee should include regular, moderate activity and weight loss, particularly in overweight and obese patients. Weight loss decreases the inflammation and joint loading that promote degeneration of the articular cartilage and is associated with decreased pain and functional impairment.
Try the UWorld AKT Question Bank for Free
Sign up for a 7-day free trial to check out the many enhanced features you’ll have immediate access to in our AKT QBank. From advanced performance analytics to integrated study tools, you’ll have everything you need to excel on exam day and during your clinical rotations.
Explore the GMC’s UKMLA AKT Question Format
The AKT exam is conducted in a multiple-choice question format based on single-best-answer questions. By incorporating realistic practice questions into your study plan, you will put yourself in the best position to succeed on the AKT.