Free Clinical Practice Questions to Maximise Your Knowledge
Sample free practice questions from our international Clinical QBank to elevate your performance in medical school and ace your exams.
UWorld Clinical QBank Sample Questions and Rationales
See for yourself why over 90% of U.S. medical students use our resources to supplement their classroom learning and prepare for their licensing exams. Answer the sample question below and experience the detailed explanations you’ll receive with every answer choice. That’s what you can expect from a full QBank subscription.
A 33-year-old woman is evaluated due to sensory loss in both upper extremities. She recently burned both of her hands while cooking but did not feel any pain. The patient has no history of trauma, headache, or neck pain. She also has no lower extremity weakness or abnormalities of bowel or bladder function. Examination shows diminished strength in the upper limbs. There is loss of pain and temperature sensation on the posterior neck, both shoulders, and both upper extremities. Vibratory and proprioceptive sensation are preserved. Which of the following is the most likely cause of this patient's symptoms?
| A. Degeneration of dorsal and lateral white matter of the spinal cord | ||
| B. Fluid-filled cavity in the central spinal cord | ||
| C. Ischemic injury of the anterior spinal cord | ||
| D. Segmental demyelination, inflammation, and gliosis of the spinal cord | ||
| E. Spondylosis, disc herniation, and spinal cord compression |
Explanation:
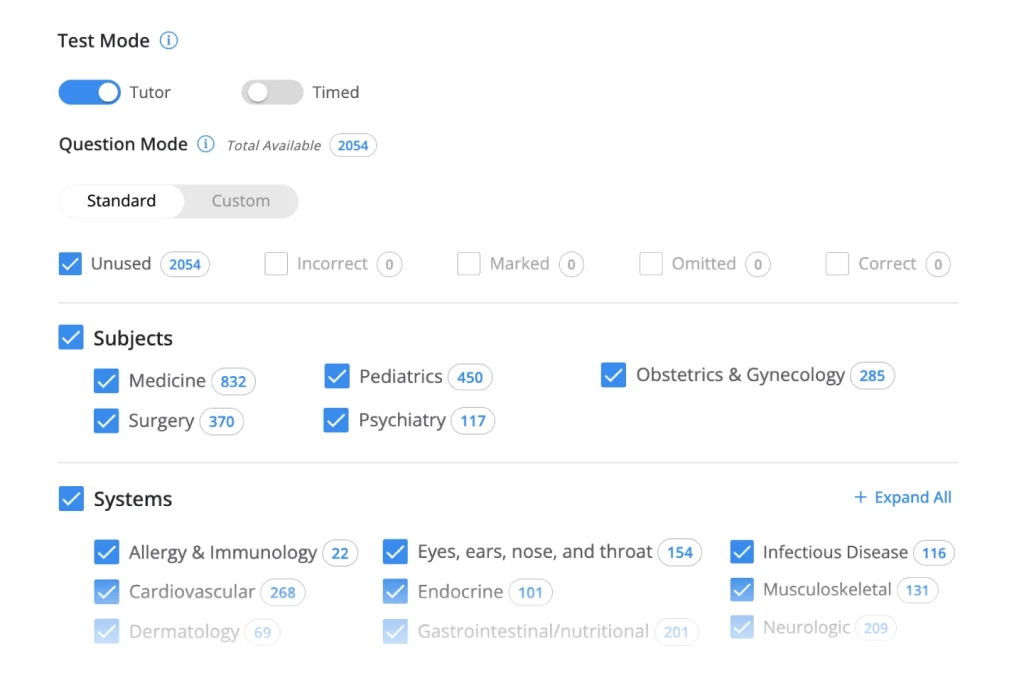
This patient likely has syringomyelia, a disorder in which a fluid-filled cavity (ie, syrinx) forms within the spinal cord. The syrinx may represent dilation of the central canal or a separate cavity within the spinal parenchyma and is usually located within the cervical or thoracic spine. Syringomyelia is most associated with Chiari type 1 malformation but may also occur with spinal cord inflammation, infection, neoplasms, or trauma.
Patients frequently have loss of pain/temperature sensation in the dermatomes corresponding to the site of spinal involvement (eg, "cape" distribution). This is due to disturbance of the crossing spinothalamic tracts (STTs) in the anterior white commissure. In contrast, vibratory/proprioceptive sensation is typically intact due to preservation of the dorsal columns (ie, dissociated sensory loss).
Continued syrinx enlargement can encroach on the central aspect of the lateral corticospinal tracts (LCTs) (in which the upper extremity fibers are somatotopically arranged more centrally) and/or the anterior horn gray matter. This produces weakness that disproportionately affects the upper extremities compared with the lower extremities.
(Choice A) Degeneration of the dorsal and lateral spinal tracts (ie, subacute combined degeneration) can occur with vitamin B12 deficiency. It typically causes impaired vibratory/proprioceptive sensation (with dorsal column involvement) and spastic muscle weakness (with LCT involvement).
(Choice C) Ischemic injury of the anterior spinal cord causes anterior cord syndrome affecting the bilateral STTs and LCTs as well as the descending autonomic tracts involved in bladder control. Anterior cord syndrome typically results in loss of pain/temperature sensation and motor function below the level of spinal injury as well as urinary incontinence.
(Choice D) Segmental demyelination/inflammation of the spinal cord (ie, transverse myelitis), as can occur in multiple sclerosis, typically presents with rapidly progressive weakness and loss of all types of sensation (eg, pain/temperature, vibratory/proprioceptive) below the level of spinal injury. Bowel and bladder dysfunction, from disruption of autonomic tracts, is common.
(Choice E) Cervical spondylosis (ie, degenerative changes of the cervical spine), which is common in elderly adults, may cause disc herniation or spinal cord compression resulting in radiculopathy and/or myelopathy. This patient's younger age and lack of neck pain make this diagnosis unlikely.
Educational objective:
Syringomyelia is a disorder in which a fluid-filled cavity forms within the spinal cord (usually within the cervical and/or thoracic spine). Patients typically have dissociated sensory loss (ie, loss of pain/temperature sensation but not vibratory/proprioceptive sensation), often in a "cape" distribution, and may develop weakness that disproportionately affects the upper extremities.
A 35-year-old man comes for evaluation of worsening shortness of breath. The patient is an avid hiker; he began to have shortness of breath 18 months ago on challenging hikes, but it now occurs even while he is walking. He has also had mild wheezing and sputum production recently. The patient has smoked half a pack of cigarettes daily for the past 5 years. His father died from lung and liver disease at a young age. Spirometry shows decreased forced expiratory volume in 1 second (FEV1), decreased forced vital capacity (FVC), and a decreased FEV1/FVC ratio. This patient's lower lung lobes are most likely to demonstrate which of the following findings?
| A. Centriacinar emphysema | ||
| B. Colonization with pathogenic bacteria | ||
| C. Compensatory hyperinflation | ||
| D. Panacinar emphysema | ||
| E. Subpleural apical blebs |
Explanation:
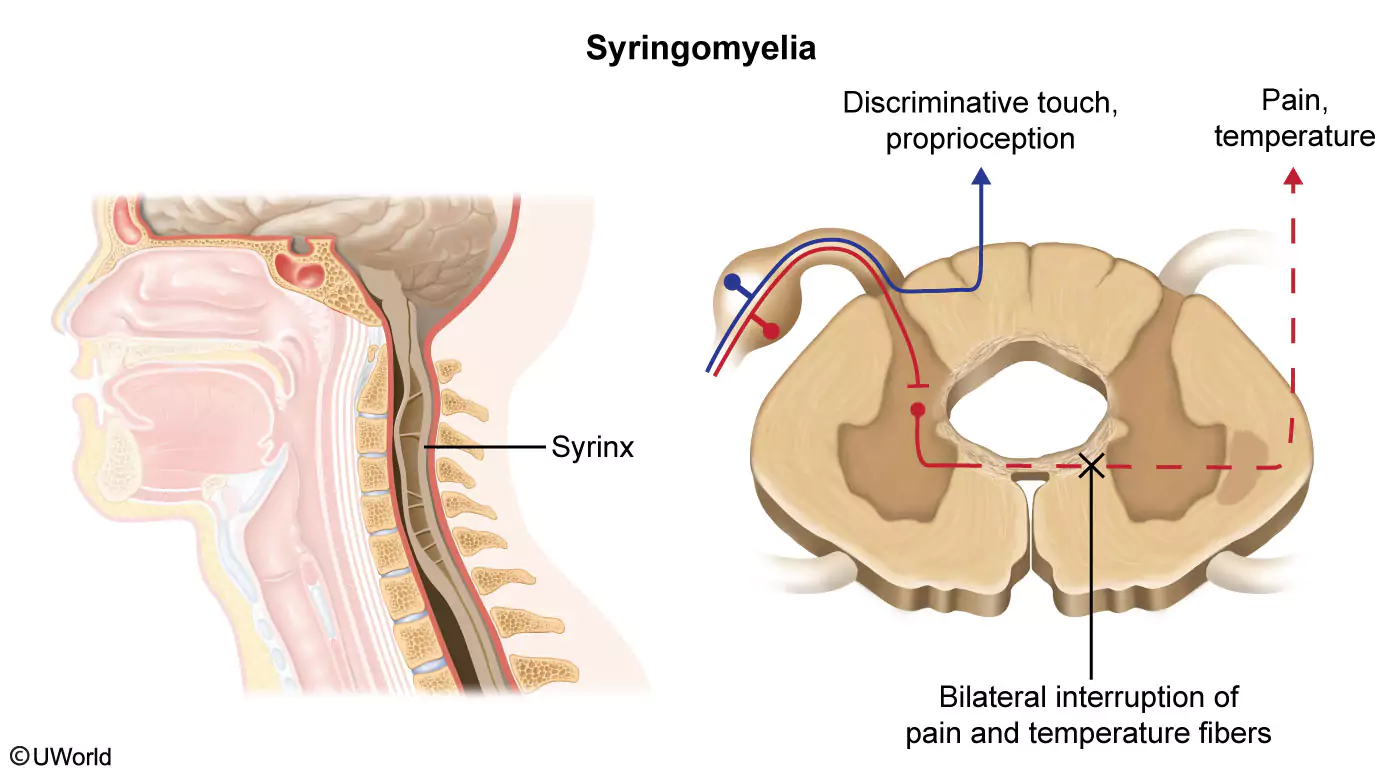
This patient with chronic progressive dyspnea has spirometry findings (reduced forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC] ratio) that are consistent with obstructive lung disease. His young age and family history of lung and liver disease suggest emphysema due to alpha-1 antitrypsin deficiency. The diagnosis is further suggested by his minimal smoking history; chronic obstructive pulmonary disease due to tobacco exposure alone is most commonly seen in those with a >30-pack-year smoking history.
Alpha-1 antitrypsin is the major inhibitor of neutrophil elastase, and deficiency leads to unchecked elastase-mediated tissue damage in the lungs, specifically panacinar emphysema. The lower lung lobes are predominantly affected, likely due to relatively greater perfusion compared to the upper lung lobes, allowing for an increased rate of neutrophil infiltration.
(Choice A) Centriacinar emphysema is characteristic of tobacco-related emphysema, as only the portion of the acinus most exposed to smoke particles is affected. Tobacco-related centriacinar emphysema predominantly affects the upper lung lobes, possibly due to a higher ventilation-perfusion ratio in those regions.
(Choice B) Colonization of the lung with pathogenic bacteria most commonly occurs in patients with cystic fibrosis and is not a common feature of alpha-1 antitrypsin deficiency.
(Choice C) Compensatory hyperinflation refers to the expansion of normal lung parenchyma that occurs when adjacent lung segments or lobes collapse or are surgically removed.
(Choice E) Subpleural blebs can develop in severe emphysema but typically occur in the apices, rather than the bases, of the lung. Their rupture is a cause of spontaneous pneumothorax.
Educational objective:
Alpha-1 antitrypsin is the major serum inhibitor of neutrophil elastase. Alpha-1 antitrypsin deficiency typically causes early-onset panacinar emphysema, predominantly affecting the lower lung lobes.
A 64-year-old man has had several episodes of intermittent hematuria over the past 2 months. He has had no abdominal pain, burning on urination, or fever but has lost 4.5 kg (10 lb) since the onset of symptoms. The patient has smoked a pack of cigarettes daily for 30 years. Vital signs are normal. The abdomen is soft, nontender, and nondistended. An enlarged and firm prostate is palpated on digital rectal examination. Serum calcium is 12.3 mg/dL (3.07 mmol/L). Urinalysis shows 30-40 red blood cells/hpf, negative protein, and no casts. A CT scan of the abdomen is shown in the exhibit. Which of the following is the most likely diagnosis?
| A. Bladder cancer | ||
| B. Pheochromocytoma | ||
| C. Polycystic kidney disease | ||
| D. Prostate cancer | ||
| E. Renal cell carcinoma |
Explanation:
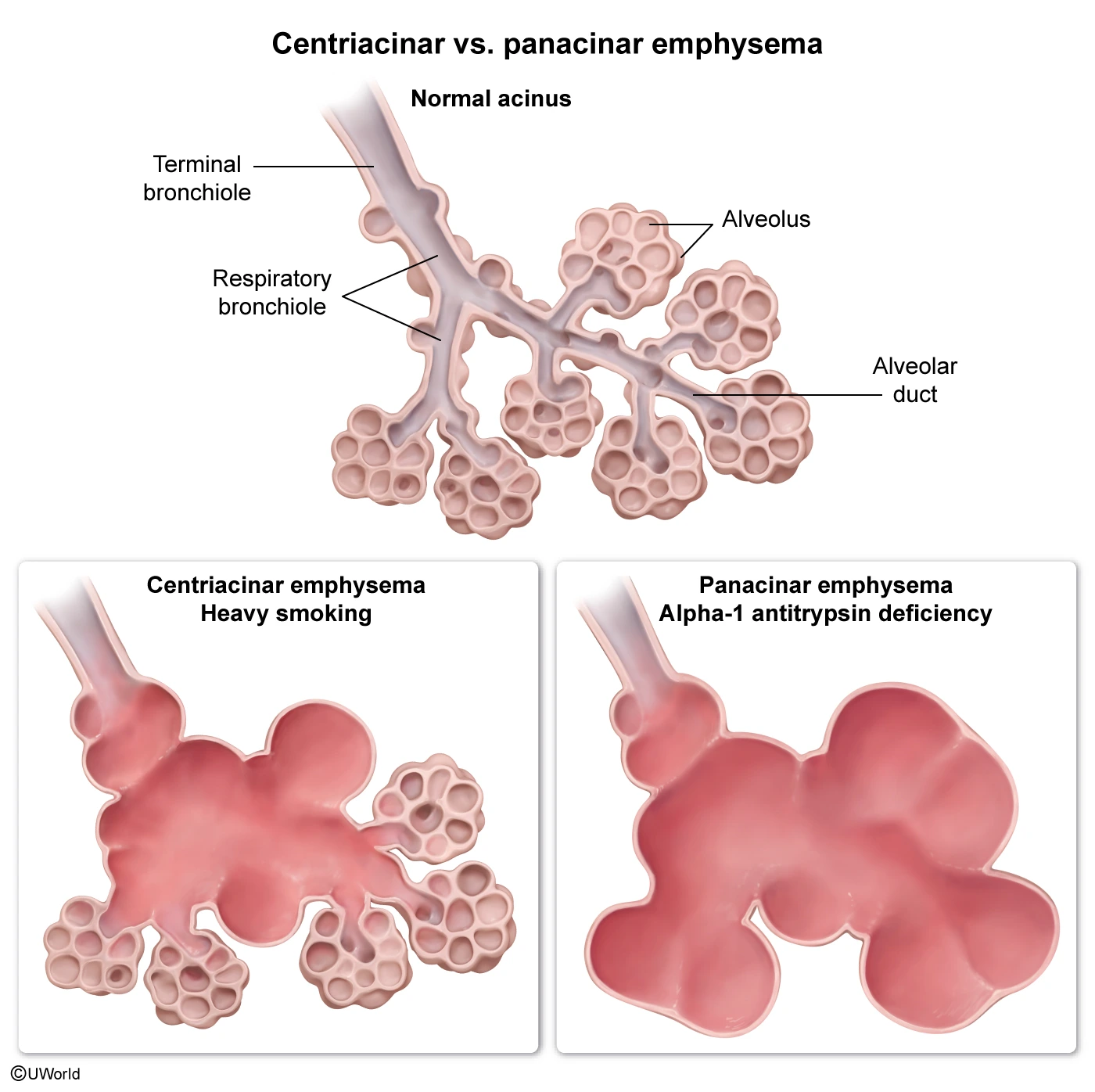
This patient with an extensive smoking history, 4.5-kg weight loss, painless hematuria, hypercalcemia, and renal mass likely has renal cell carcinoma (RCC). RCC originates in the renal cortex and accounts for up to 90% of primary renal tumors. It is often identified incidentally on radiographic imaging, and many individuals remain asymptomatic until the disease is relatively advanced. Hematuria is the most common symptom, and painless hematuria in an adult should raise suspicion for a genitourinary malignancy. Patients may also have flank pain and a palpable abdominal mass at the time of presentation.
Paraneoplastic syndromes are common in RCC due to the secretion of biologically active substances by the tumor cells. Hypercalcemia is frequently seen due to increased production of parathyroid hormone–related peptide or overproduction of prostaglandins that promote bony resorption. Erythrocytosis (due to ectopic erythropoietin production) and hepatic dysfunction unrelated to liver metastases may also be seen.
(Choice A) Bladder cancer is another common cause of hematuria and weight loss; however, CT scan would demonstrate a bladder mass. This malignancy tends to metastasize to the liver, bones, and lungs, not the kidney. Although hypercalcemia may occur occasionally, it is more strongly associated with RCC.
(Choice B) Pheochromocytoma can cause severe, episodic hypertension associated with headaches, anxiety, palpitations, and sweating. A CT scan would reveal a suprarenal mass, and urine catecholamines and metanephrines would be elevated. Hematuria is not seen.
(Choice C) Polycystic kidney disease can cause hematuria; however, flank pain is common, and imaging would show bilateral renal cysts, not a unilateral mass. In addition, weight loss and hypercalcemia would be unexpected.
(Choice D) Prostate cancer typically presents with discrete nodules or asymmetric induration of the prostate on digital rectal examination. Diffuse, symmetric enlargement and firmness of the prostate are more suggestive of benign prostatic hyperplasia.
Educational objective:
Classic signs and symptoms of renal cell carcinoma (RCC) include hematuria, an abdominal mass, flank pain, and weight loss. Hypercalcemia and erythrocytosis are common paraneoplastic syndromes associated with RCC.
A 64-year-old man with a history of coronary artery disease and peripheral vascular disease undergoes coronary artery bypass surgery. His postoperative course is complicated by hypotension, which is treated successfully with intravenous fluids; however, a few hours later, he experiences abdominal pain followed by bloody diarrhea. Temperature is 37.8 C (100 F), blood pressure is 110/60 mm Hg, and pulse is 110/min. Abdominal examination shows normal bowel sounds, with no significant guarding or focal tenderness. A venous lactic acid level is elevated. An abdominal CT scan is ordered. Which of the following areas will most likely show abnormal findings?
| A. Ascending colon | ||
| B. Hepatic flexure | ||
| C. Jejunum | ||
| D. Mid transverse colon | ||
| E. Splenic flexure |
Explanation:
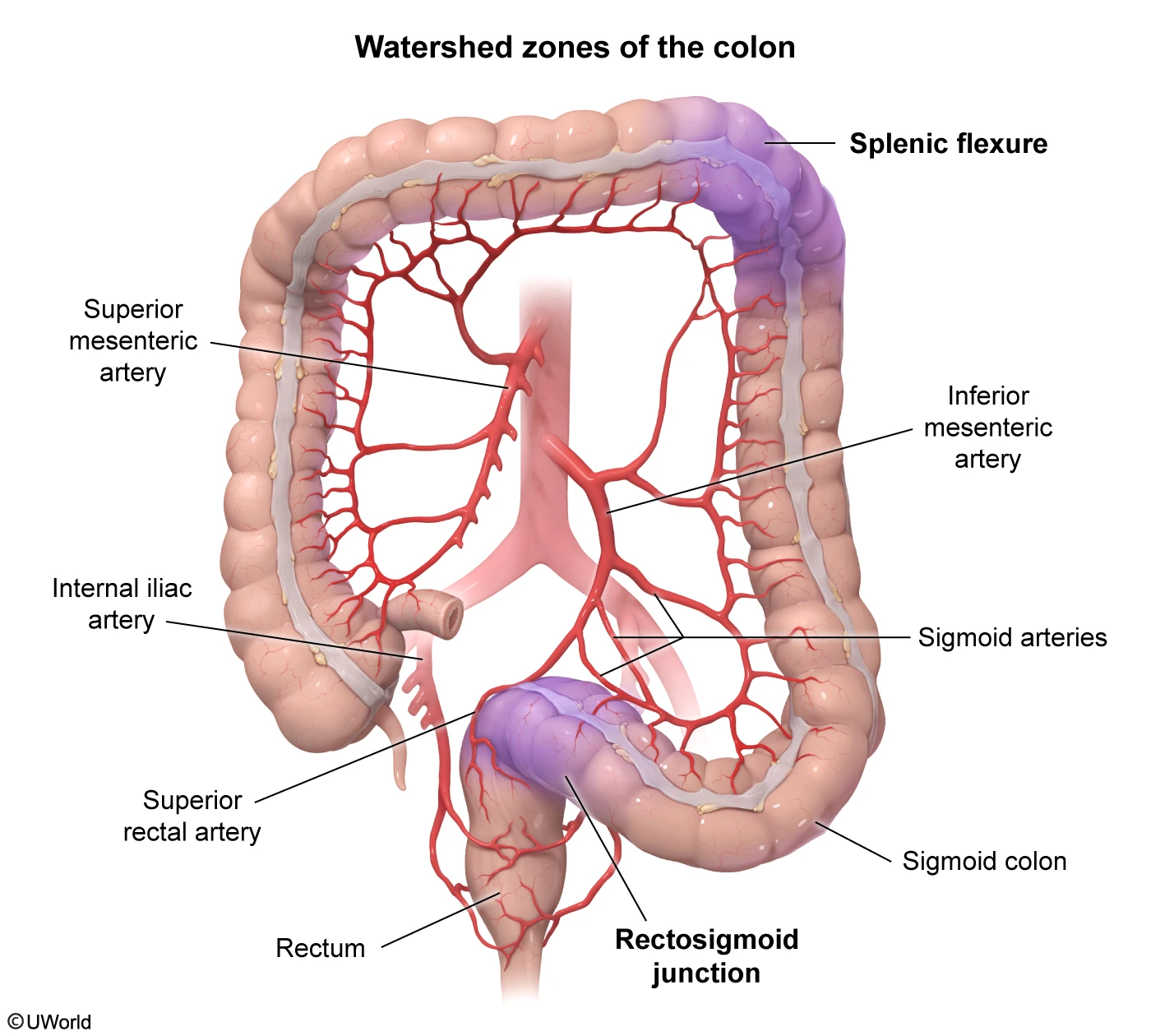
This patient with acute abdominal pain followed by lower gastrointestinal bleeding after an episode of hypotension most likely has ischemic colitis. Fever, nausea, elevated lactic acid, and leukocytosis may also be seen. Older patients with atherosclerotic vascular disease are at particularly high risk. The most commonly involved segments of the colon include the splenic flexure at the "watershed" line between the territory of the superior and inferior mesenteric arteries and the rectosigmoid junction at the watershed between the sigmoid artery and superior rectal artery.
Abdominal CT scan with intravenous contrast may show thickened bowel wall, although it may demonstrate only nonspecific findings. CT should be performed urgently to identify patients with ischemic colitis who need immediate surgical intervention (eg, extensive bowel damage, perforation). If colon resection is not needed, patients are treated with intravenous fluids and antibiotics and endoscopic evaluation (colonoscopy) is performed to confirm the diagnosis. Typical findings include pale mucosa with petechial bleeding, bluish hemorrhagic nodules, or cyanotic mucosa with hemorrhage.
(Choices A, B, and D) The ascending colon, hepatic flexure, and mid transverse colon are singularly supplied, and, therefore, not considered watershed areas at high risk for ischemia.
(Choice C) Small bowel (mesenteric) ischemia is usually due to atheroembolic (eg, endovascular procedures) or thromboembolic (eg, atrial fibrillation) events rather than acute hypotension. Pain is typically severe but is poorly localized and out of proportion to examination findings; hematochezia may occur but is a late finding. CT would show focal or segmental bowel wall thickening and mesenteric stranding.
Educational objective:
Ischemic colitis is characterized by acute abdominal pain and lower gastrointestinal bleeding. It typically follows an episode of hypotension and most commonly affects arterial watershed areas at the splenic flexure and rectosigmoid junction. CT scan may show a thickened bowel wall. Colonoscopy can confirm the diagnosis.
A 3-year-old boy woke up with a sore throat this morning and has been refusing to eat. Temperature is 38.7 C (101.7 F) and respirations are 28/min. The patient is sitting still and appears scared. He has a hoarse voice, rhinorrhea, and mild stridor. The posterior pharynx has no erythema or tonsillar exudate. The anterior neck is tender to palpation. Lung examination reveals transmitted upper airway sounds that are equal bilaterally without crackles or wheezes. Lateral neck x-ray is shown in the exhibit. Which of the following is the most likely diagnosis?
| A. Bacterial tracheitis | ||
| B. Croup | ||
| C. Epiglottitis | ||
| D. Peritonsillar abscess | ||
| E. Retropharyngeal abscess |
Explanation:
Epiglottitis is a rare, potentially fatal infection that presents with acute onset of fever, sore throat, and signs of upper airway obstruction (eg, stridor, drooling). Symptoms often develop over hours without a notable prodrome, as seen in this patient. Impending signs of respiratory failure include anxiety, worsening stridor, and a muffled/hoarse, "hot potato" voice. Patients may display tripod positioning (leaning forward, neck hyperextension) to maximize airway diameter. The anterior neck near the hyoid bone may be tender, and oropharyngeal examination is typically normal other than pooled oral secretions.
X-ray is not required for diagnosis if clinical suspicion is high, but lateral view shows an enlarged epiglottis (thumb sign), suggestive of edema. Diagnosis is confirmed via direct visualization of an edematous epiglottis. However, detailed oropharyngeal examination is often deferred in children due to risk of laryngospasm from provoked aggravation. Direct laryngoscopy during intubation (a controlled setting to secure the airway) is often preferred for diagnosis and management.
(Choices A and B) Bacterial tracheitis presents with fever, stridor, and respiratory distress. Croup presents with a "barky" cough, hoarseness, stridor, and fever. In both conditions, onset is gradual (over days), and neck x-ray (posterioanterior view) reveals subglottic narrowing (eg, steeple sign) and a normal epiglottis. This patient has a thickened epiglottis on x-ray, a finding consistent only with epiglottitis.
(Choice D) Peritonsillar abscess is most common in older children and adolescents; it presents with gradual onset of fever, muffled voice, and unilateral tonsillar swelling with uvular deviation. This patient's age, normal oropharyngeal examination, and acute symptom onset make this diagnosis unlikely.
(Choice E) Retropharyngeal abscess presents with fever, dysphagia, drooling, stridor, and a stiff neck in young children. Examination reveals swelling of the posterior pharyngeal wall (not seen in this case), and x-ray shows widening of the retropharyngeal space, not a thickened epiglottis.
Educational objective:
Epiglottitis is a rare but potentially fatal infection that presents with acute onset of fever, sore throat, and signs of upper airway obstruction (eg, stridor, drooling). Plain x-rays may help confirm the diagnosis by revealing an enlarged epiglottis (thumb sign).
Try the UWorld Clinical QBank for Free
Instantly access 25 free practice questions and answer explanations for 7 days, with no credit card required! Get a first-hand look at our custom flashcards, digital notebook, and reporting tools.
Improve Your Clinical Understanding
The UWorld Clinical QBank is a self-study resource for medical students planning to practise outside the United States. It consists of 2,000+ practice questions tailored to standard universal medications and requirements and features our detailed answer explanations trusted by 2+ million students.
Learn from
Medical Experts
Retain Difficult
Concepts Faster
Connect Theory
to Practise
Is the Clinical QBank Right for You?
Most UWorld QBanks are country- or exam-specific. The Clinical QBank focuses on the standard medications and requirements doctors around the world need to know to safely and effectively practise medicine.
High-Yield Clinical MCQs for Medical Students Everywhere
The Clinical QBank provides you with a proven self-study resource regardless of your location. Each question is written in a simplified, single-best-answer format and paired with a visually engaging rationale that walks you through the problem. Learn from realistic scenarios to enhance your classroom learning and prepare for your career.
Prepare with the Clinical QBank from Anywhere
Access your full Clinical QBank and favourite learning tools anywhere you have an internet connection with the UWorld Medical app. Adapt your study sessions to your schedule and conveniently pick up where you left off. Simply sign in with your account to get started.
Frequently Asked Questions
The UWorld Clinical QBank covers universal medications and requirements based on standard Subjects and Systems to improve your clinical judgement. While the material will not fully align with your specific exam’s content outline, it can be used as a supplement to your medical school curriculum and licensing exam preparation.
Yes. The UWorld Clinical QBank was created to help medical students improve their performance in the classroom, during rotations, and on their licensing exams. It features realistic clinical scenarios to help you connect your classroom learning to real-life practise.
If you plan to become a doctor in the United States, you will need to pass all 3 sections of the United States Medical Licensing Examination® (USMLE®). If this is your goal, you should consider our USMLE QBanks, which are trusted by over 90% of U.S. medical students.
The UWorld Clinical QBank comes with 2,000+ practice questions that cover the topics you can expect to learn in medical school. While every student’s needs are different, we suggest completing all of our questions in alignment with your school curriculum to maximise your understanding.
Our team of practising doctors and medical educators continually reviews and updates your QBank content to ensure it remains relevant. Any changes are made automatically.