Free COMLEX® Sample Questions for Levels 1 and 2
Try free UWorld questions for your COMLEX® Level 1 or Level 2 exam to test your knowledge and see if our QBank is right for you.
Why Choose Our COMLEX Questions?
Practice Quizzes
on Test Day
to Your Needs
Try Our OMT-Style Questions for Level 1 and Level 2
A 17-year-old boy comes to the emergency department due to a right ring finger injury earlier in the day. During a soccer match, he grabbed an opponent's jersey; as the opponent pulled away suddenly, the patient instantly felt a popping sensation and pain in the right ring finger. Examination of the hand shows swelling of the palmar aspect of the distal ring finger. When asked to make a fist, the patient can flex the metacarpophalangeal and proximal interphalangeal joints but is unable to flex the distal interphalangeal joint of the ring finger. The tendon of which of the following muscles is most likely injured in this patient?
- Flexor carpi ulnaris
- Flexor digitorum profundus
- Flexor digitorum superficialis
- Fourth lumbrical
- Palmar interosseous
Explanation:
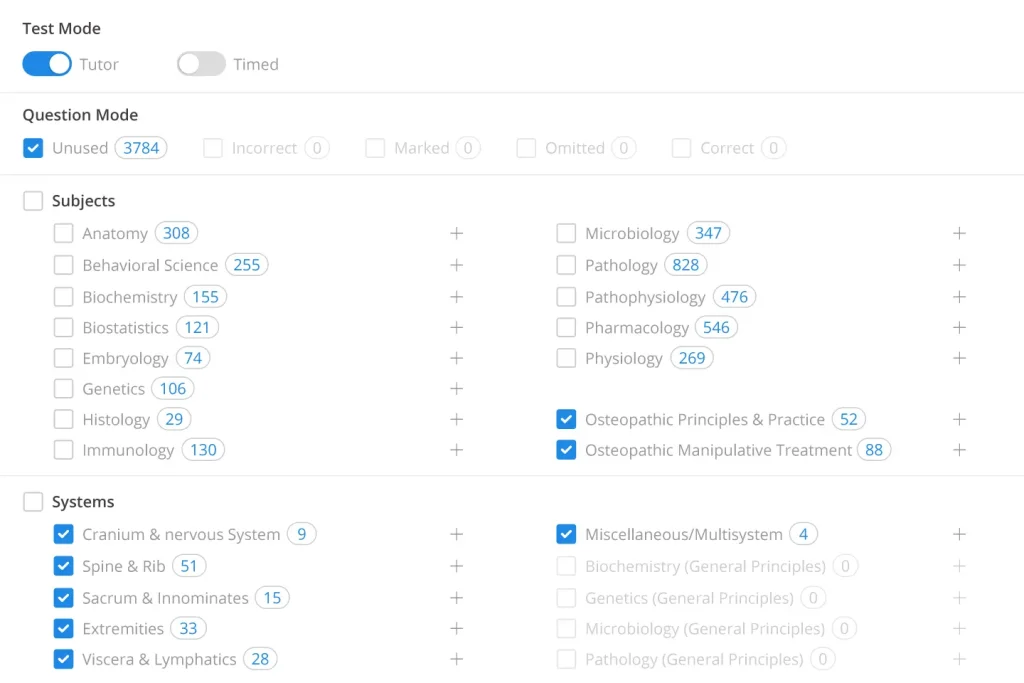
This patient who felt a popping sensation in his right finger while grabbing another player's jersey has likely ruptured the flexor digitorum profundus (FDP) tendon, an injury commonly called "jersey finger."
The FDP tendon originates from the FDP muscle in the forearm; travels through the carpal tunnel, palm, and flexor tendon sheath; and inserts onto the base of the distal phalanx. It contributes to flexion of proximal joints (wrist, metacarpophalangeal [MCP] joint, proximal interphalangeal [PIP] joint) and specifically causes flexion of the distal interphalangeal (DIP) joint. It is typically weakest at its insertion and is susceptible to rupture when the actively flexed DIP joint (eg, hooked around opponent's jersey) is forcefully hyperextended (eg, opponent pulls away suddenly). Rupture can occur in any digit, but the ring finger is most frequently involved.
Patients with FDP tendon rupture commonly have pain and swelling in the affected digit. A complete tendon rupture, as seen in this patient, results in absent DIP flexion; a partial tendon tear results in weak, incomplete flexion.
(Choice A) The flexor carpi ulnaris (FCU) is a primary flexor of the wrist. FCU tendon injury results in decreased wrist flexion power; some wrist flexion is maintained by the other wrist flexors (eg, flexor carpi radialis).
(Choice C) The flexor digitorum superficialis (FDS) tendon inserts onto the body of the middle phalanx; it does not contribute to DIP joint flexion.
(Choice D) The lumbrical muscles are intrinsic muscles of the hand that contribute to MCP joint flexion and interphalangeal joint extension. Injury to the fourth lumbrical tendon would decrease these functions in the small finger where the fourth lumbrical tendon inserts.
(Choice E) The palmar interosseous muscles are intrinsic muscles of the hand that adduct the fingers and, in coordination with the dorsal interossei, assist in MCP joint flexion and interphalangeal joint extension. Tendon injury would primarily decrease finger adduction.
Educational objective:
The flexor digitorum profundus tendon inserts onto the base of the distal phalanx and flexes the distal interphalangeal (DIP) joint. It is susceptible to rupture when an actively flexed DIP joint is forcefully hyperextended.
A 25-year-old man fractures his right tibia in a motor vehicle collision. His right leg is fixed in a cast, and he requires underarm crutches to ambulate. Two weeks later, the patient comes to the clinic with right upper extremity weakness and numbness. He has no neck or arm pain. The patient is concerned because he is right handed and cannot perform his duties as an electrician. On neurologic examination, there is diminished strength on extension of the right wrist with an absent triceps reflex. Injury to which of the following nerves is most likely responsible for this patient's symptoms?
- Accessory
- Axillary
- Long thoracic
- Median
- Radial
- Suprascapular
Explanation:
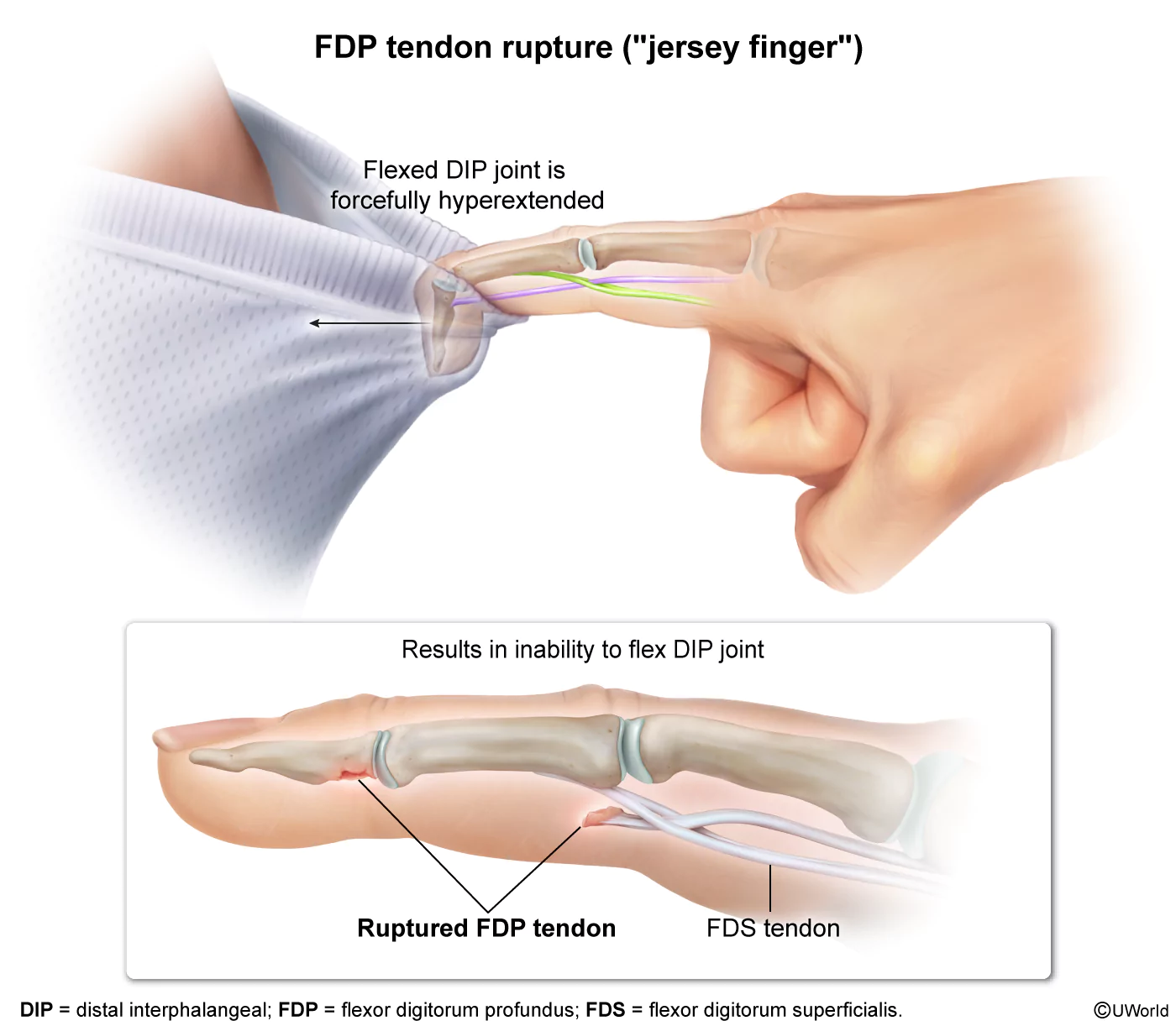
The radial nerve is derived from the C5-T1 spinal nerves and is 1 of the 2 final branches of the posterior cord of the brachial plexus. The nerve initially courses medial to the surgical neck of the humerus inferior to the teres major muscle within the axilla before entering the posterior arm to course between the long head of the triceps brachii and the posterior humerus.
Proximal radial nerve injury can occur at the nerve's superficial location within the axilla by repetitive pressure/trauma caused by an ill-fitting crutch (crutch palsy) or if an individual sleeps with the arm over a chair (Saturday night palsy). Injury at this location may cause weakness or paralysis of the forearm, hand, and finger extensor muscles (eg, wrist drop, absent triceps reflex). Sensory loss may also be observed over the radial nerve distribution.
Injuries to the radial nerve as it crosses the posterior humerus (eg, midshaft humeral fractures) spare the triceps brachii, as the fibers innervating this muscle leave the nerve before entering the radial groove.
(Choice A) The accessory nerve (CN XI) exits the skull through the jugular foramen and courses over the levator scapulae muscle to innervate the sternocleidomastoid and trapezius muscles. Injury to CN XI can occur during cervical lymph node dissection.
(Choice B) Fracture of the surgical neck of the humerus and anterior dislocation of the glenohumeral joint can cause injury to the axillary nerve. The resultant paralysis of the deltoid and teres minor muscles causes weakness on arm abduction. Sensory loss over the deltoid may also be evident.
(Choice C) Damage to the long thoracic nerve causes paralysis of the serratus anterior muscle and winging of the scapula. This nerve is often injured during axillary lymph node dissection in patients undergoing radical mastectomy.
(Choice D) Proximal median nerve injury often occurs with supracondylar humerus fractures. This results in sensory loss over the palmar aspect of the first 3 digits and impairment of thumb flexion/opposition, flexion of the second/third digits, and wrist flexion/abduction.
(Choice F) The suprascapular nerve provides sensation to the shoulder joint and innervates the supraspinatus and infraspinatus muscles. Suprascapular nerve entrapment results in shoulder pain and weakness of arm abduction and external rotation.
Educational objective:
Radial nerve injury can occur with repetitive pressure/trauma at the axilla (eg, improperly fitted crutches). Findings include weakness of the forearm, hand, and fingers extensors (eg, wrist drop, absent triceps reflex) and sensory loss over the posterior arm and forearm, dorsolateral hand, and dorsal thumb. More distal lesions spare the triceps brachii.
A 27-year-old female comes to the office for right shoulder pain. The pain started 2 weeks ago while she was assembling furniture. Despite using ice packs and taking nonsteroidal anti-inflammatory drugs several times per day for the past week, the pain is now interfering with her sleep and her job as an operating room technician. She has no significant medical history and takes no medications. Vital signs are normal. Physical examination shows tenderness to palpation over the anterior aspect of the right shoulder at the bicipital groove. C6 is flexed, rotated right, sidebent right (FRSR). To perform a provocative test that will aid in the diagnosis of this patient, the physician should
- Have the patient externally rotate her shoulder against resistance
- Place the patient's hand on her back and have her push back against resistance
- Resist abduction of the patient's adducted arm
- Resist adduction of the patient's abducted arm
- Supinate and extend the patient's forearm
Explanation:
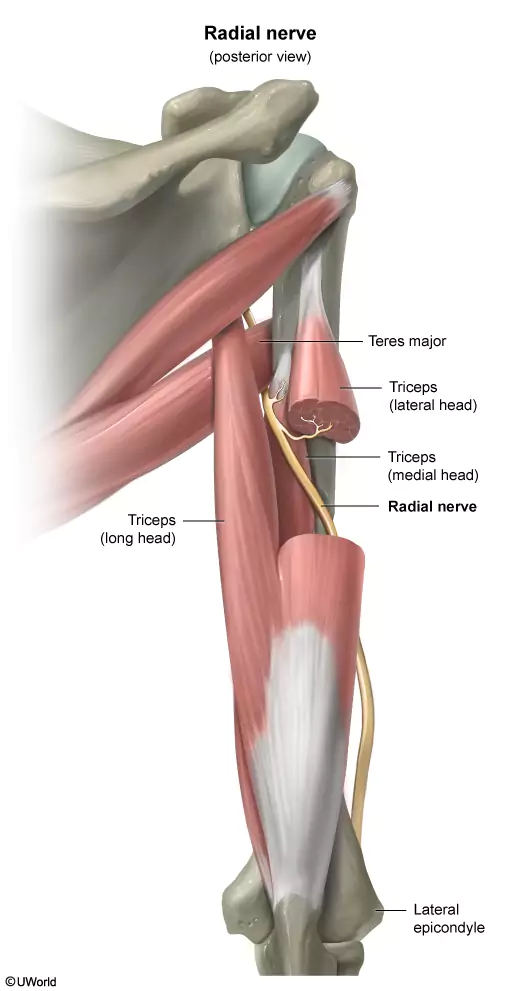
This patient with localized anterior right shoulder pain and tenderness at the bicipital groove likely has bicipital tendonitis. This inflammatory and degenerative disorder is initiated by injury or microtrauma of the long head of the biceps tendon in the bicipital groove due to overuse and/or chronic tendon subluxation. The pain is often localized to the anterior shoulder over the bicipital groove but can also radiate down into the biceps.
Provocative tests that can assist in the evaluation of these patients include the following:
- Yergason test: assesses for pain and/or instability of the biceps tendon while supinating and extending the patient's forearm (with the elbow initially flexed 90 degrees).
- Biceps squeeze test: assesses the integrity of the biceps tendon by evaluating for supination while squeezing the patient's biceps firmly.
- Speed test: assesses the biceps tendon by having the patient flex his or her arm past 90 degrees against resistance with the forearm extended and supinated.
Initial treatment of bicipital tendonitis consists of rest, nonsteroidal anti-inflammatory drugs, physical therapy, and osteopathic manipulative treatment for associated somatic dysfunctions (eg, C6 FRRSR). If the pain is persistent or severe, ultrasound-guided glucocorticoid injection into the sheath of the long head of the biceps tendon at the bicipital groove can improve function and decrease pain.
(Choices A, B, and C) Rotator cuff function/integrity can be assessed by flexing the patient's arm at the elbow before having the patient externally rotate her shoulder against resistance (infraspinatus, teres minor), placing the patient's hand on the back and having the patient push back against resistance (subscapularis), and having the patient abduct the arm against resistance (supraspinatus). Rotator cuff tendinopathy typically presents with pain over the upper/posterolateral (rather than anterior) shoulder that is worse with overhead movements.
(Choice D) Adducting the arm across the torso against resistance increases compression at the acromioclavicular (AC) joint. AC joint disease presents with tenderness over the AC joint (rather than the bicipital groove).
Educational objective:
Bicipital tendonitis is caused by inflammation of the long head of the biceps tendon within the bicipital groove and presents with anterior shoulder pain. Extending and supinating the patient's forearm (ie, Yergason test) is one of the provocative maneuvers that can aid in diagnosis.
A 31-year-old female is evaluated for left knee pain that started 3 months ago while she was running a half-marathon. Physical examination shows slight tenderness over the lateral knee without effusion or erythema. The McMurray and Ober tests are negative. Squatting and compression of the patella do not elicit pain. There is restriction in left foot dorsiflexion and eversion. The best next step in management of this patient is
- Exercises to strengthen the vastus medialis
- HVLA for anterior fibular head dysfunction
- Muscle energy for posterior fibular head dysfunction
- Physical therapy for iliotibial band syndrome
- Steroid injection for prepatellar bursitis
Explanation:
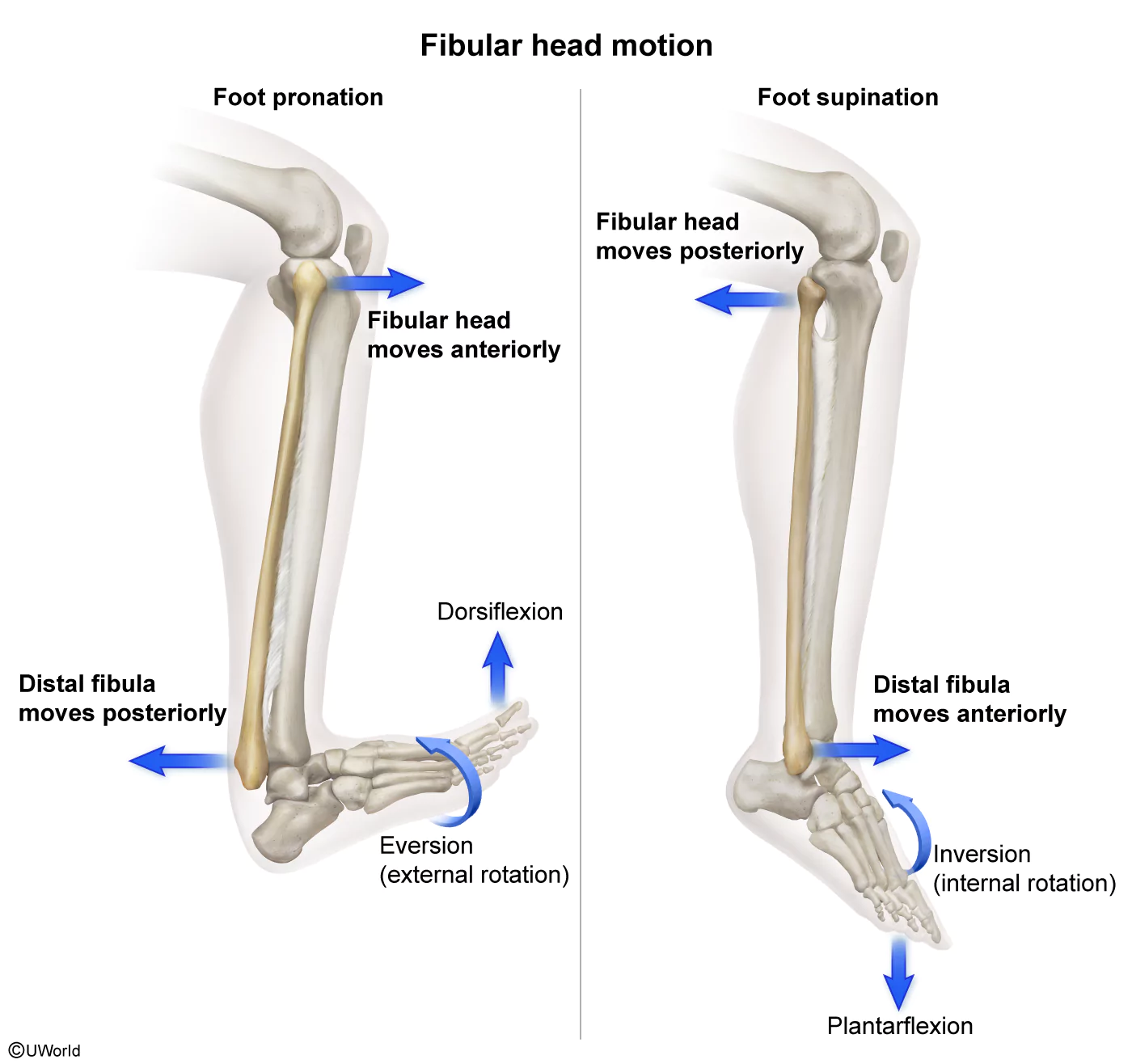
This patient with left knee pain, restriction in foot pronation (ie, dorsiflexion and eversion) and tenderness over the lateral knee likely has a fibular head dysfunction. During foot pronation and supination, movement of the distal fibula at the ankle and the proximal fibula (ie, fibular head) at the knee occurs in opposite directions (ie, reciprocal motion):
- Foot pronation (ie, dorsiflexion and eversion/external rotation) pushes the distal fibula posteriorly. Because the distal fibula is linked to the fibular head (ie, proximal fibula) via the interosseous membrane, this results in anterior glide of the fibular head.
- Foot supination (ie, plantarflexion and inversion/internal rotation) pulls the distal fibula anteriorly, resulting in posterior glide of the fibular head.
This patient's restriction in foot pronation (dorsiflexion and eversion/external rotation) indicates that the foot is "stuck" in the supinated (plantarflexed and inverted/internally rotated) position with the distal fibula displaced anteriorly and the fibular head "stuck" posteriorly (ie, posterior fibular head dysfunction) (Choice B).
Muscle energy (direct) restores normal motion by moving the fibular head that is "stuck" posteriorly through the restrictive barrier to anterior glide. To perform muscle energy for posterior fibular head dysfunction:
- The physician positions the fibular head against the restrictive barrier by pushing anteriorly on the posterior aspect of the fibular head and everting/externally rotating the foot.
- The patient then attempts to invert/internally rotate the foot against resistance (ie, isometric contraction).
- This stimulates Golgi tendon organs, which initiate muscle relaxation (ie, postisometric relaxation), allowing movement through the restrictive barrier (to anterior glide) into a neutral position.
(Choice A) Patellofemoral syndrome is characterized by anterior knee pain caused by patellar malalignment. It presents with anterior knee pain that is worse while running, squatting, or negotiating stairs. Treatment consists of quadriceps strengthening exercises specifically targetting the vastus medialis muscle.
(Choice D) Although iliotibial band syndrome also causes lateral knee pain and is also common in runners, physical examination typically shows a positive Ober test (physician stretches the iliotibial band by flexing the knee and abducting the leg) without restriction in foot pronation or supination.
(Choice E) Although inflammation of the bursae overlying the patella (ie, prepatellar bursa) causes knee pain, the pain is located anteriorly rather than laterally. There is also associated localized swelling, exquisite tenderness, and erythema.
Educational objective:
Posterior fibular head dysfunction presents with restriction of anterior glide of the fibular head, resulting in restricted foot pronation (ie, dorsiflexion and eversion/external rotation). Muscle energy helps move the fibular head (which is "stuck" posteriorly) through the restrictive barrier to anterior glide.
A 65-year-old male is being evaluated for back pain. The pain is dull and radiates down his right leg and foot. It first started 7 months ago and has been worsening progressively despite taking acetaminophen and using lidocaine patches. The patient does not remember any injury or event that first caused the pain but reports that the symptoms seem to be worse when he works in his garden. Vital signs are normal. Physical examination shows increased pain on lumbar extension and diminished sensation over the anterior left lower leg and dorsal foot. Strength is normal in both lower extremities. L2-L4 are flexed, rotated left, sidebent left (FRLSL). This patient's sensory loss best correlates with compression of nerve roots that exit between
- T11-T12
- L1-L2
- L3-L4
- L5-S1
Explanation:
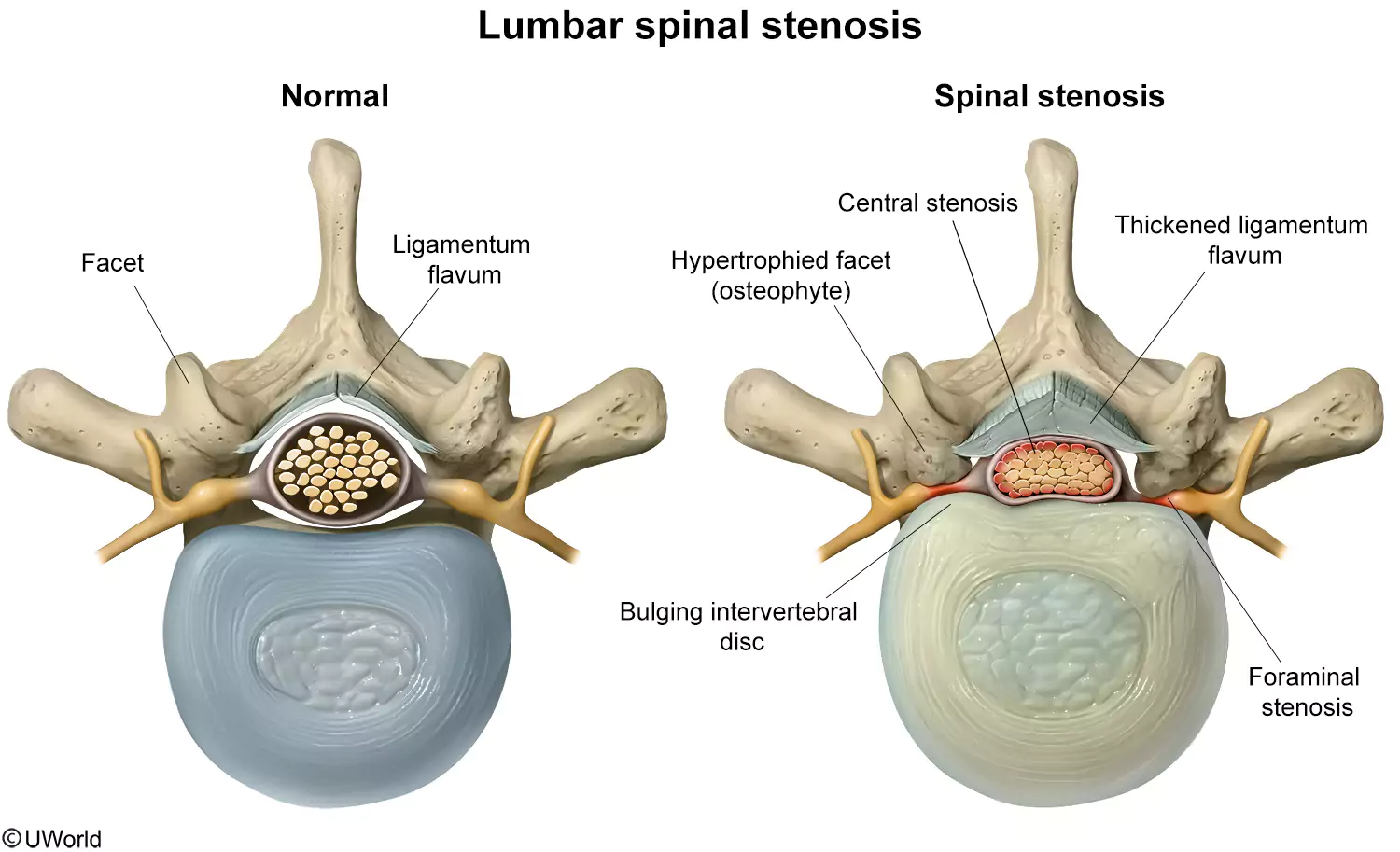
This patient's progressive low back pain and sensory loss are likely due to spinal stenosis, an abnormal narrowing of the spinal canal and/or intervertebral foramen. In spinal stenosis, there is formation of facet joint osteophytes and hypertrophy of the ligamentum flavum, which can compress spinal nerve roots. Patients have chronic back pain radiating down the lower extremities, numbness/paresthesia, and occasionally weakness. Symptoms are worsened with lumbar extension, which further narrows the spinal canal, and are relieved with lumbar flexion (ie, leaning on a stroller/shopping cart).
Spinal stenosis typically affects the nerve root of the corresponding vertebral level as it exits the intervertebral foramen. This patient's sensory loss of the anterior lower leg and dorsal foot (ie, L5 dermatome ) suggests compression of the L5 nerve root as it exits the intervertebral foramen between L5 and S1. Spinal stenosis is treated with physical therapy and nonsteroidal anti-inflammatory drugs/muscle relaxants. Surgical laminectomy may be helpful in refractory cases.
Lumbar somatic dysfunctions are commonly seen in patients with spinal stenosis (due to compensatory changes). Because lumbar extension exacerbates pain, patients naturally spend more time with the lumbar spine flexed, which can cause flexion dysfunctions (eg, L2-L4 FRLSL as in this patient). Osteopathic manipulative treatment can help improve overall function and mobility, although it will not address the underlying degenerative changes.
(Choices A, B and C) Although spinal stenosis can occur at these levels, the dermatomal distribution of the radicular pain would not involve the anterior lower leg and dorsal foot, as in this patient.
Educational objective:
Spinal stenosis results from degenerative changes that narrow the spinal canal and/or intervertebral foramen. Narrowing of the intervertebral foramen at L5-S1 compresses the L5 nerve root, causing radiating pain, numbness, and/or paresthesia of the anterior lower leg and dorsal foot.
A 38-year-old male is evaluated in the emergency department for right arm pain and swelling. He injected intravenous heroin 3 days ago into the antecubital fossa and noticed erythema surrounding the injection site the following day. Vital signs show:
| Temperature | 38.8 C (101.8 F) |
| Blood pressure | 144/80 mm Hg |
| Heart rate | 105/min |
| Respiratory rate | 15/min |
| Oxygen saturation | 98% on room air |
Physical examination shows erythema, tenderness, and warmth of the right antecubital fossa with an underlying 1 x 1 cm fluctuant mass. Lymphatic drainage from the affected region primarily drains into the junction of which of the following structures?
- Left brachiocephalic and internal jugular veins
- Left brachiocephalic vein and superior vena cava
- Right brachiocephalic vein and superior vena cava
- Right internal jugular and subclavian vein
Explanation:
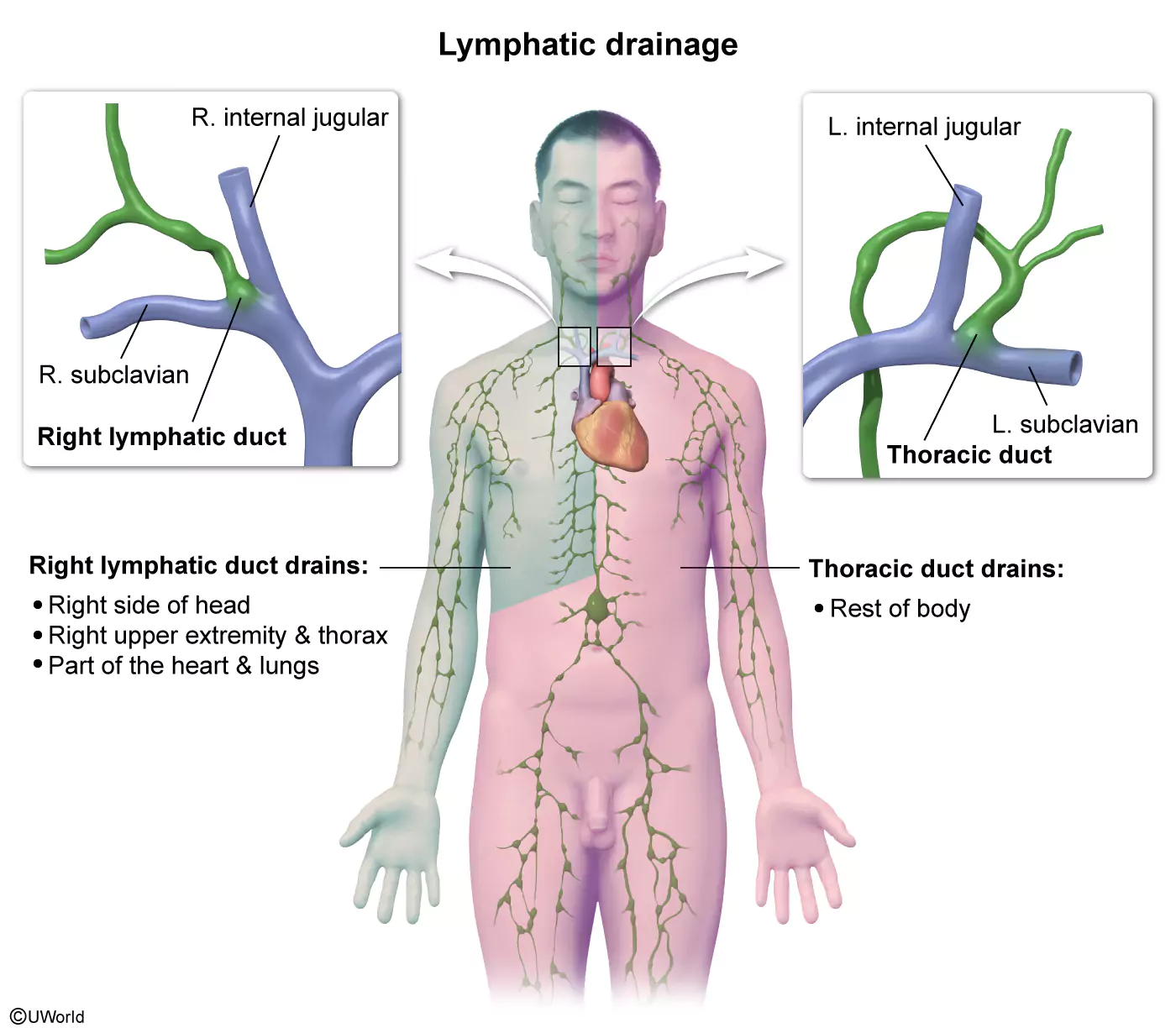
This patient with fever has physical examination findings indicating a right arm abscess with surrounding cellulitis precipitated by intravenous drug use. Erythema, tenderness, and warmth are a manifestation of the inflammatory response that is mediated by the immune system in response to localized infection. Lymphatic fluid containing a mixture of immune cells and bacteria (and their byproducts) from the right upper extremity drains into the right lymphatic duct. The right lymphatic duct ultimately drains into the venous circulation.
The right lymphatic duct (ie, right/minor thoracic duct)
- Receives drainage from the right upper extremity, right side of the head, part of the heart and lungs, and the right thorax
- Drains into the junction of the right internal jugular and right subclavian vein (which combine to form the right brachiocephalic vein).
In contrast, the thoracic duct (ie, left/major thoracic duct)
- Receives drainage from the remainder of the body (including both lower extremities).
- Drains into the junction of the left internal jugular vein and left subclavian vein, which combine to form the left brachiocephalic vein (Choice A).
The left and right brachiocephalic veins combine to form the superior vena cava, which drains into the right atrium (Choices B and C).
Educational objective:
The right (minor) thoracic duct carries lymphatic fluid from the right upper extremity, right side of the head, part of the heart and lungs, and the right thorax. It drains into the junction of the right internal jugular and subclavian veins (which combine to form the right brachiocephalic vein).
Your All-In-One Exam Prep Resource
Our COMLEX QBanks give you everything you need to pass your licensing exams and excel in your career.
- Level 1: 3,600+ Step 1 questions and 140+ OMT questions for preclinical success
- Level 2: 4,250+ Step 2 CK questions, 140+ OMT questions, and a dedicated shelf review interface
COMLEX Success Stories
Frequently Asked Questions (FAQs)
Do UWorld COMLEX questions meet NBOME requirements?
No. Our OMT questions offer COMLEX-style vignettes to prepare you for what you’ll see on test day, but do not comprehensively cover the NBOME exam blueprints. However, our USMLE QBanks do adhere to each NBME content outline.
How many COMLEX sample questions do I need to practice?
We recommend starting early and completing as many questions as you can reasonably accomplish before your exam. Begin by studying about 30 minutes per day and build to 20 questions per day. The goal is to take in the information and avoid overloading yourself. Try to complete a full pass of your QBank before dedicated study and then another during it.
Is there a free trial for UWorld COMLEX QBanks?
No. We do not offer a free trial for the OMT questions in our COMLEX QBanks. However, you can access free 10-question demos of our USMLE QBanks, which are available in combination with our OMT questions.