Free ABFM® and ABIM® Sample Questions
Try free UWorld questions for your family medicine or internal medicine board exam to test your knowledge and see if our QBank is right for you.
Why Choose Our Medical Board Exam Questions?
Study the Topics Most Relevant to You
Improve Your Confidence on Exam Day
Learn from Premier Answer Explanations
Try Our ABFM and ABIM Questions
A 1.9 kg (4.2 lb) boy is born by vaginal delivery to a 27-year-old woman who had no prenatal care. The boy's mother is not sure when her last menstrual period was or when she became pregnant. Maternal serologies are drawn and the mother is found to be hepatitis B surface antigen positive. The remainder of her hepatitis panel is pending. The infant is well-appearing.
Which of the following is the most appropriate next step in the management of this infant?
- Administer hepatitis B immune globulin now, and vaccine once infant is >2 kg (4.4 lb)
- Administer hepatitis B vaccine and immune globulin if mother is hepatitis B e-antigen positive
- Administer hepatitis B vaccine and immune globulin now
- Administer hepatitis B vaccine now
- Administer hepatitis B vaccine now, and immune globulin if mother is hepatitis B e-antigen positive
Explanation:
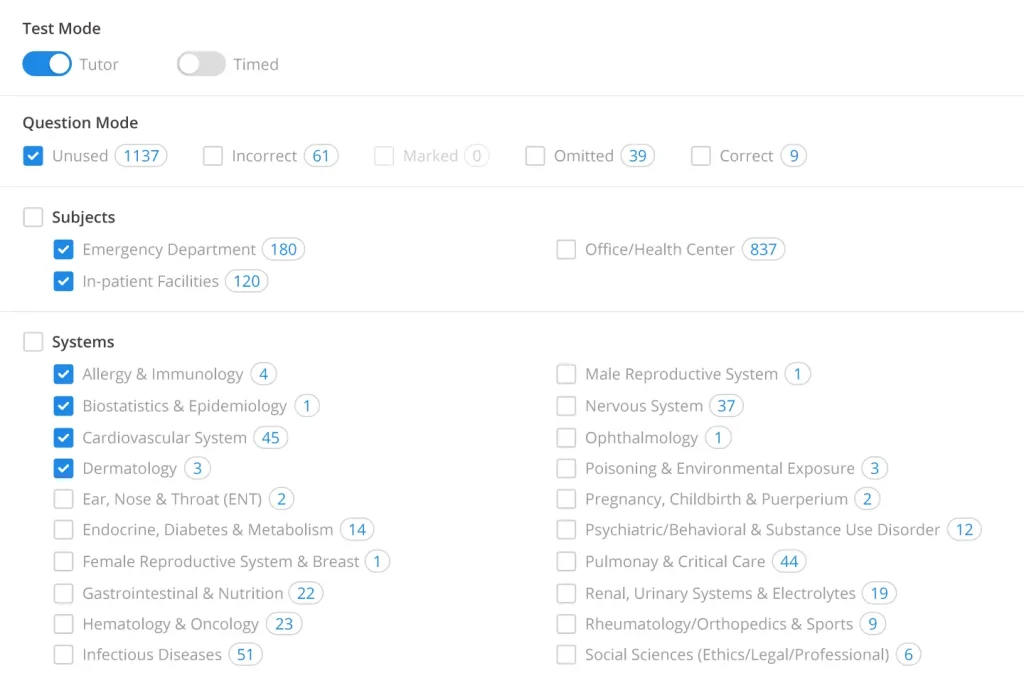
Hepatitis B infection can be transmitted to newborns at delivery (exposure to infectious genital secretions) or in utero via transplacental infection. Preterm infants and infants born to mothers who are hepatitis B e-antigen (HBeAg) positive have the highest risk. More than 90% of hepatitis B infections acquired in infancy will become chronic.
Prevention of mother-to-child transmission of hepatitis B is best achieved by screening all pregnant women for hepatitis B surface antigen (HBsAg). HBsAg+ mothers require a full panel to determine their disease stage and personal risk, but the full serology panel is not needed to manage their infants. Infants born to HBsAg+ mothers should receive hepatitis B immune globulin (HBIG) and hepatitis B vaccine (HBV) as soon as possible regardless of their birth weight or gestational age. These infants should be followed closely and should have serologic testing at age 9-15 months to determine whether they are infected.
(Choice A) HBV is delayed until age 30 days or hospital discharge for infants <2 kg (4.4 lb) at birth, unless they were exposed to maternal hepatitis B virus. Infants who are born to HBsAg+ mothers, as in this case, should receive HBV and HBIG immediately regardless of their birth weight.
(Choices B and E) Infants born to mothers with detectable HBeAg have the highest risk for infection. However, the risk for perinatal infection is ~20% even if the mother is HBeAg negative. Therefore, all infants born to HBsAg+ mothers should be treated with HBIG and HBV immediately, without waiting on any further testing.
(Choice D) Active immunization with HBV is important, but it is not sufficient protection in post-exposure cases. HBV should be combined with HBIG for all infants exposed to the maternal hepatitis B virus.
Educational objective:
All infants born to mothers with positive hepatitis B surface antigen testing should receive hepatitis B immune globulin and hepatitis B vaccine as soon as possible after delivery. This treatment should be given regardless of the infant's gestational age, birth weight, or other maternal serologies.
A 15-year-old boy comes to the clinic with 4 days of worsening cough and fever and 1 day of rash. The cough is nonproductive and has not interfered with school attendance or basketball practice. The patient has no medical problems and takes no medications. His immunizations are up to date, including the seasonal influenza vaccination. The patient's temperature is 38.7 C (101.7 F), and respiratory rate is 24/min. Pulse oximetry shows 97% on room air. Examination shows a well-appearing boy with bilateral crackles and wheezes. A diffuse rash is seen on his trunk and extremities. The remainder of the physical examination is unremarkable.
Which of the following is the most appropriate next step in management of this patient?
- Amoxicillin
- Azithromycin
- Chest x-ray
- Corticosteroids
- Oseltamivir
Explanation:
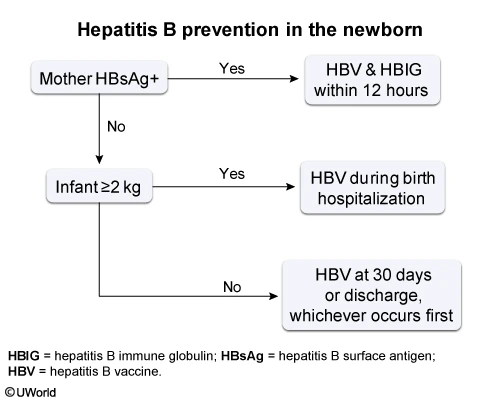
This patient's cough, fever, and adventitious noises on chest examination are consistent with pneumonia. The bilateral lung findings and wheezing suggest an atypical process rather than a lobar pneumonia. Mycoplasma pneumoniae is the most common cause of atypical pneumonia in patients age >5. M pneumoniae infections are associated with complications, such as hemolytic anemia and mucocutaneous lesions. The erythematous target-shaped rash on this patient's skin is consistent with erythema multiforme.
First-line therapy for Mycoplasma infection is oral azithromycin. A 5-day course (10 mg/kg/day on day 1 followed by 5 mg/kg/day on days 2-5) is generally effective. If the patient does not begin to improve within 48 hours, macrolide resistance should be suspected and therapy with doxycycline or levofloxacin may be warranted.
(Choice A) M pneumoniae lacks a cell wall and is therefore resistant to amoxicillin. However, if lobar pneumonia (most commonly due to Streptococcus pneumoniae) cannot be excluded, then combination therapy with azithromycin and amoxicillin is appropriate.
(Choice C) Chest x-rays are reserved for dyspneic or hypoxic patients to assess pneumonia severity and possible complications (eg, empyema, effusion). It is not necessary in patients with a characteristic examination who can be managed as outpatients.
(Choice D) Systemic corticosteroids may be used to treat a severe asthma exacerbation, but they are not indicated for atypical pneumonia or erythema multiforme. Erythema multiforme can be treated symptomatically with anti-inflammatory agents and topical steroids, but systemic steroids have been associated with progression to Stevens-Johnson syndrome. Treating the underlying trigger (in this case, infection) is the best way to treat erythema multiforme.
(Choice E) Influenza can cause pneumonia and erythema multiforme and can be treated with oseltamivir. However, viral lower respiratory tract disease is uncommon in children age >5, and this patient is at even lower risk due to his influenza vaccination.
Educational objective:
Mycoplasma pneumoniae is the most common cause of atypical pneumonia in patients age >5. It should be suspected in a patient with bilateral pneumonia and extrapulmonary findings, such as hemolytic anemia or mucocutaneous lesions. Azithromycin is the treatment of choice.
A 62-year-old woman comes to the physician due to right knee pain and swelling for the last 6 months. The pain is worse with activity and better with rest. She does not use tobacco, alcohol, or illicit drugs. Her mother had rheumatoid arthritis. The patient's temperature is 37.2 C (98.9 F), and blood pressure is 146/86 mm Hg. Her BMI is 34 kg/m2. Examination shows a mild effusion, tenderness, and decreased range of motion of the right knee. Synovial fluid analysis reveals the following:
| White blood cell count | 1100/mL |
| Gram stain | negative |
| Crystals | absent |
Which of the following is most likely to be found on x-rays of the knee?
- Calcifications of cartilaginous structures
- Narrowing of joint space and osteophyte formation
- Normal joint space with soft tissue swelling
- Periarticular osteopenia and joint margin erosions
- Punched-out erosions with a rim of cortical bone
Explanation:
This patient's clinical features – chronic knee pain, decreased range of motion, bland synovial effusion - are most consistent with osteoarthritis (OA). OA is a noninflammatory arthritis that most commonly affects the hands and weight-bearing joints. Patients typically report mild morning stiffness (<30 minutes) and pain that is exacerbated by exercise and relieved by rest. Unlike autoimmune arthropathy (eg, rheumatoid arthritis), systemic symptoms are absent. Effusions may occur in OA but the joint will remain cool to the touch. Joint crepitus, bony enlargement, and painful or decreased range of motion are also common.
Synovial fluid analysis typically shows a white blood cell (WBC) count of 200-2000/mL (as opposed to 0-200/mL in a normal joint, 2,000-50,000/mL in inflammatory arthritis, and >50,000/mL in septic arthritis). Plain films often reveal a narrowed joint space with osteophyte formation. Other possible findings include subchondral sclerosis/cysts.
(Choice A) Calcification of cartilaginous structures (chondrocalcinosis) is typical of pseudogout, or calcium pyrophosphate dihydrate (CPPD) deposition. Symptoms include acute swelling, stiffness, and pain of the knee. Synovial fluid demonstrates a WBC count of 2,000-50,000/mL with rhomboid, positively birefringent crystals.
(Choice C) Normal joint space with soft tissue swelling is seen on radiography in patients with infectious arthritis. WBC count of >50,000/mL is typical on synovial fluid analysis and the Gram stain often shows bacteria.
(Choice D) Periarticular osteopenia and joint margin erosions suggest rheumatoid arthritis (RA), which is characterized by prolonged morning stiffness (especially in the wrists and metacarpophalangeal and proximal interphalangeal joints), fever, malaise, and weight loss. The joints will be warm and doughy to the touch, with a WBC count of 2,000-50,000/mL on fluid analysis.
(Choice E) Punched-out erosions with a rim of cortical bone are the characteristic x-ray finding in gouty arthritis. Gout causes acute joint pain, and synovial fluid analysis will demonstrate a WBC count of 2,000-50,000/mL and needle-shaped, negatively birefringent crystals.
Educational objective:
Osteoarthritis is a non-inflammatory arthritis causing pain that is worse with activity and improved with rest. X-ray findings include joint space narrowing and osteophytes. Synovial fluid analysis will reveal a white blood cell count <2000/mL, no organisms, and no crystals.
A 46-year-old man comes to the physician because of recurrent abdominal discomfort. He describes episodes of moderate, dull, epigastric pain lasting 2-3 days that have occurred 1-2 times/month over the last 2 years. He also describes occasional nausea but denies any vomiting, diarrhea, black stools, blood in the stool, abdominal distention, or weight loss. He takes ibuprofen for chronic low back pain. He drinks 8-10 beers over the weekends and frequently throughout the week.
His vital signs are within normal limits and his BMI is 28 kg/m2. Physical examination is unremarkable.
Fasting blood glucose is 127 mg/dL. Abdominal x-ray shows focal calcifications anterior to the spine over the epigastric area.
Upper GI endoscopy reveals a normal esophagus, gastric varices in the fundus of the stomach, and a normal duodenum.
Which of the following is the most likely diagnosis?
- Alcoholic liver cirrhosis
- Gastroparesis
- Helicobacter pylori infection
- Non-ulcer dyspepsia
- Splenic vein thrombosis
Explanation:
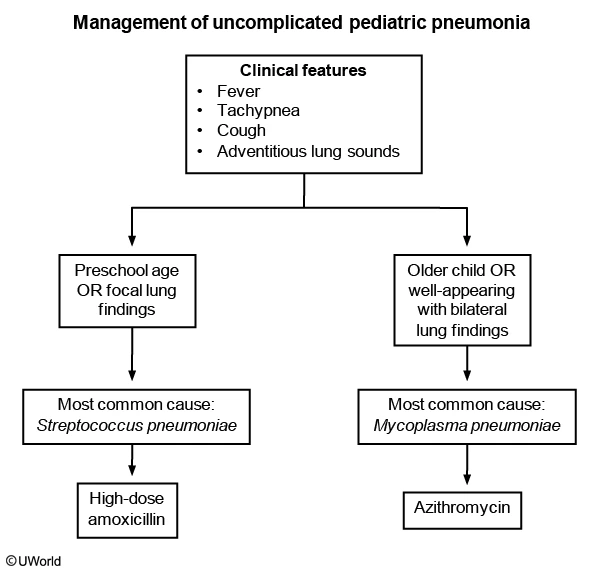
This patient’s presentation is consistent with chronic pancreatitis due to excessive alcohol intake. Abdominal x-rays typically show calcifications in the area of the pancreas. The splenic vein runs along the posterior surface of the pancreas, where chronic pancreatic inflammation can lead to thrombosis. Splenic vein thrombosis leads to gastric varices near the gastric fundus only; esophageal varices are not seen. Variceal hemorrhage is the most common symptom of splenic vein thrombosis and splenectomy is usually curative.
(Choice A) Cirrhosis causes scarring in the liver that leads to increased sinusoidal vascular pressures and portal hypertension. These patients typically present with esophageal varices, diffuse gastric varices (not just gastric fundus), and rectal varices (hemorrhoids).
(Choice B) Gastroparesis is usually a complication of diabetes (rather than chronic pancreatitis) and causes delayed gastric emptying. Patients typically present with nausea/vomiting and bloating, and endoscopy will not show varices.
(Choice C) Helicobacter pylori is a common cause of ulcer disease and may be associated with dyspepsia. This patient’s use of alcohol and NSAIDs increases his risk of peptic ulcer disease, but his endoscopy showing varices make this less likely.
(Choice D) Non-ulcer dyspepsia is usually diagnosed after excluding other etiologies (e.g., peptic ulcer disease, GERD, and malignancy). However, this patient’s abnormal endoscopy showing varices makes this unlikely.
Educational objective:
Chronic pancreatitis can lead to splenic vein thrombosis. Gastric varices localized to the gastric fundus confirm the diagnosis. Bleeding from these varices can be cured by splenectomy.
A 55-year-old man is evaluated for acute onset of respiratory distress. He was admitted to the hospital after a highway traffic accident, which resulted in a left femur and wrist fracture. He was immediately taken to the operating room and underwent open reduction and internal fixation. The total blood loss was estimated at 1.1 liters and he was given 2 liters of intravenous normal saline and one unit of packed red blood cells intraoperatively. He was extubated and transferred to the postoperative recovery room. One hour following extubation, he developed acute respiratory distress requiring reintubation. His other medical problems include inferior wall myocardial infarction with right coronary artery stent placement 3 years ago, hypertension, hyperlipidemia, and type 2 diabetes mellitus. His home medications include aspirin, metoprolol, lisinopril, metformin, and rosuvastatin.
His temperature is 38.1 C (100.6 F), blood pressure is 110/70 mm Hg, pulse is 110/min, respirations are 30/min, and oxygen saturation is 90% on 100% FiO2 and 10 mm Hg of PEEP. He is drowsy from the sedation and intravenous hydromorphone infusion. There is no jugular venous distention or lower extremity edema. Pulmonary examination reveals diffuse crackles throughout the lungs. There are no heart murmurs. Skin examination reveals no rashes.
Arterial blood gas shows a pH of 7.47, PaCO2 of 32 mm Hg, and PaO2 of 65 mm Hg.
ECG shows sinus tachycardia. His preoperative chest x-ray was within normal limits. Repeat chest x-ray taken before reintubation is shown below.
Which of the following is the most likely cause of his current condition?
- Anaphylactic transfusion reaction
- Aspiration pneumonia
- Fat embolism
- Transfusion-associated acute lung injury
- Volume overload
Explanation:
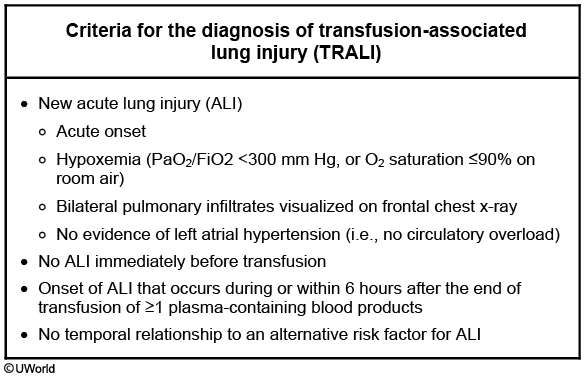
This patient’s presentation is consistent with transfusion-related acute lung injury (TRALI). Plasma is most frequently responsible for TRALI, but packed red blood cells, platelets, and other blood derivatives have also been implicated. Transfusion-related acute lung injury is likely due to anti-leukocyte antibodies from the donor's plasma reacting with antigens on the recipient's leukocytes to initiate an inflammatory response within the pulmonary microvasculature.
Patients with TRALI usually present with sudden onset dyspnea, hypoxemia, and pulmonary infiltrates during or within 6 hours of any blood product transfusion (in the absence of circulatory overload). Chest x-ray shows bilateral patchy alveolar infiltrates consistent with ARDS. Importantly, TRALI diagnosis requires that patients not have preexisting ALI or other established ALI risk factors (e.g., septic shock, pneumonia, inhalation injury, etc.).
Management of TRALI involves immediately stopping the transfusion, providing respiratory support (sometimes intubation), and vasopressors for hypotension. Clinical improvement occurs rapidly, even with severe hypoxemia, and most patients are extubated within 2 days. Patients with TRALI should receive no further plasma-containing blood products from the implicated donor. In addition, the blood bank should be notified and the donor investigated to prevent future incidents to other transfusion recipients from the donor. Patients recovering from TRALI are not at a significantly increased risk for recurrent episodes following transfusions from other donors.
(Choice A) Anaphylactic transfusion reaction (more common in patients with IgA deficiency) presents with a rapid onset of dyspnea, stridor, wheezing, respiratory distress, and hypotension. However, anaphylactic transfusion reaction is not usually associated with abnormal chest x-ray findings, as seen in this patient.
(Choice B) Aspiration pneumonia usually presents with cough, fever, purulent sputum, and dyspnea. However, symptoms usually evolve over a period of time. Aspiration pneumonitis (acid chemical pneumonitis) can cause acute distress and infiltrates but is rarely severe enough to cause florid ARDS. Infiltrates are typically localized to one or both lower lobes.
(Choice C) The probability of fat embolism syndrome (FES) with a single long bone fracture is 1-3%; this increases to 33% with bilateral femur fractures. Fat embolism syndrome usually presents with the clinical triad of acute-onset neurologic abnormalities (e.g., confusion), hypoxemia, and petechial rash. FES typically manifests 24-72 hours after the initial insult and usually with a normal chest x-ray in the majority of patients.
(Choice E) Transfusion-associated circulatory overload (TACO) usually presents with physical findings suggesting volume overload (e.g., elevated JVD, presence of an S3). Measurement of serum brain natriuretic peptide (BNP) or NT-Pro-BNP can also help in distinguishing TRALI from TACO. This patient received approximately 2.5 liters of fluid and has had 1.1 liters of blood loss, making volume overload unlikely.
Educational objective:
Transfusion-related acute lung injury (TRALI) should be considered in patients with acute onset dyspnea, hypoxemia, and pulmonary infiltrates that occur during or within 6 hours after transfusion of any plasma containing blood product. Treatment involves mainly supportive care, stopping the transfusion, and vasopressor support for hypotension. The blood bank should be notified and the blood donor investigated to prevent future incidents in other recipients.
A 65-year-old woman comes to the physician with a pruritic rash. This is the second year the rash has appeared, both times during the onset of winter. She has intensely pruritic areas on her lower extremities along the shins and above the right lateral malleolus. The patient sometimes experiences pruritus on her lower back and the extensor surfaces of the forearms. One area usually predominates. There is no visible rash initially, but the involved areas can become rough and scaly after a few weeks of frequent scratching. Her only other medical problem is perennial rhinitis. Her medications include cetirizine, calcium plus vitamin D supplements, and a multivitamin.
Skin examination findings are shown in the photograph.
Which of the following is the best next step in management of this patient?
- Capsaicin ointment
- Comprehensive metabolic panel and thyroid-stimulating hormone
- Moisturizing agent
- Skin biopsy
- Topical terbinafine
Explanation:
This patient's presentation of dry, scaly, itchy, and red skin is consistent with skin dryness (xerosis). Xerosis ('winter itch') is more common in the winter months due to dry weather. The elderly (who have decreased sebaceous/sweat gland activity) and patients who bathe frequently or take offending medications (eg, doxycycline) are at particularly high risk. The dry skin can easily become irritated, leading to pruritus and excoriations. One or a few areas are usually involved and systemic pruritus is not present. Patients eventually develop thickened and scaly lichenified plaques in pruritic areas. Areas not within reach of the hands are typically not involved.
Most cases can be managed with daily skin moisturizers and topical emollients. Patients should also use gentle cleansers (eg, moisturizing bar soaps) and lukewarm (rather than hot) water when bathing. Other alleviating treatments include lotions (eg, calamine, menthol-containing) for cool skin relief, reducing possible skin irritants, using a humidifier in the winter, and stress reduction. More advanced cases may require topical corticosteroids.
(Choice A) Capsaicin is derived from chili peppers and can be effective for neuropathic (eg, notalgia paresthetica, brachioradial pruritus) and certain pruritic conditions (eg, prurigo nodularis, aquagenic pruritus, pruritus associated with chronic renal disease). However, it is not as effective for xerosis.
(Choice B) Generalized pruritus due to systemic causes requires further investigation, including thyroid-stimulating hormone, creatinine, bilirubin, calcium, and blood glucose levels. However, this patient's seasonal symptoms and localized pruritus make this less likely.
(Choice D) Xerosis is usually a clinical diagnosis and requires a skin biopsy only in cases with unclear etiology.
(Choice E) Topical terbinafine is effective for tinea corporis, a fungal infection that usually presents with ringlike papulosquamous eruptions on the arms and legs.
Educational objective:
Xerosis is dry skin due to depleted moisture that results in intensely pruritic areas. Recurrent excoriation of the area can expand the lesion and lead to lichenification. Most cases can be managed with daily skin moisturizers and topical emollients.
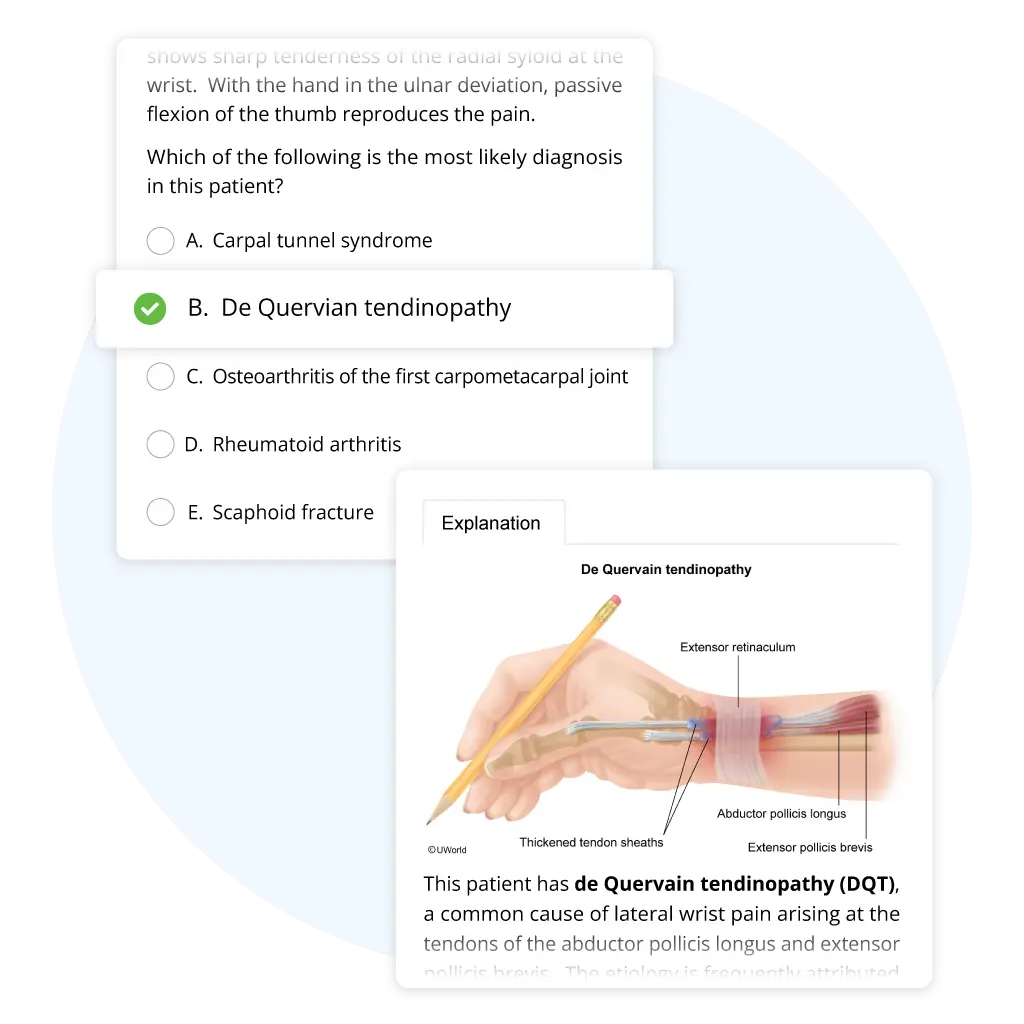
Make the Real Exam Feel Like Practice
We give you the tools you need to study your way and broaden your understanding of tested concepts.
- Prepare with realistic exam questions written by board-certified doctors and internists.
- Visualize scenarios with detailed answer explanations that contain images of symptoms, flowcharts, and tables.
- Read a brief statement outlining the educational objective of each question, and gain further insights through links to PubMed.
Study Your Boards Material from Anywhere
Finding time to prepare for your medical board exam can be difficult. That’s why our ABFM and ABIM questions and study tools can be fully accessed from the UWorld Medical app. Simply sign in to your account to get started — available for Apple and Android tablets and smartphones.
ABFM and ABIM Success Stories
Frequently Asked Questions (FAQs)
Do UWorld questions meet ABFM and ABIM content requirements?
Yes. Our ABFM QBank adheres to the latest American Board of Family Medicine exam blueprint, and our ABIM QBank adheres to the latest American Board of Internal Medicine exam blueprint. We mirror each exam’s testing interface and question types to deliver a realistic practice environment.
How is UWorld boards content different from other materials?
Our question style, content coverage, and testing interface are most similar to the actual exam to ensure you’re ready on test day. We also offer a number of active learning tools and performance metrics to give you greater control over your prep. With UWorld, you’ll get all the basics you need to build a strong foundation of knowledge and pass your board exam.
How many boards sample questions should I practice?
We recommend completing our full QBank to ensure you’ve adequately reviewed each exam topic. However, we understand that your work schedule may make that difficult. We include a variety of subscription durations, study tools, and performance metrics to help you optimize your efforts.
Is there a free trial for UWorld Medical board exam QBanks?
No. We do not offer free trials for our ABFM or ABIM QBanks. However, we do offer 10-question demos to give you a look at our user interface and available study tools.