Juvenile Idiopathic Arthritis
Article Sections
Introduction
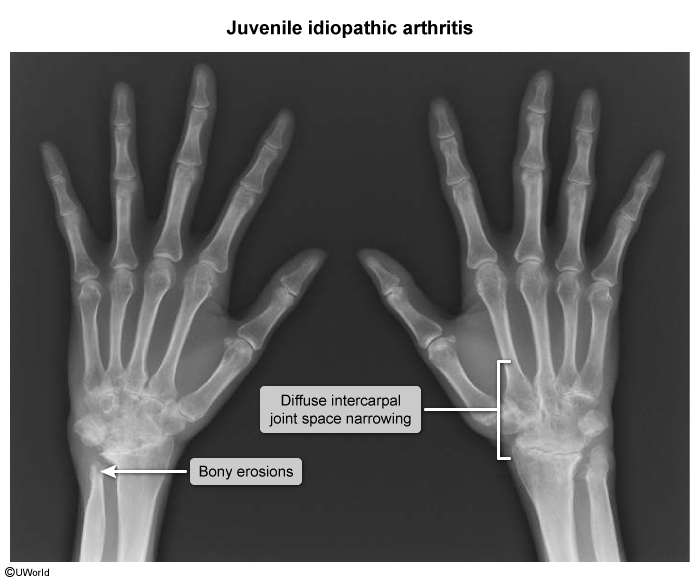
Juvenile idiopathic arthritis (JIA) is a chronic idiopathic autoinflammatory condition that primarily involves the joints. The diagnosis comprises systemic, polyarticular, and oligoarticular subtypes, each with its own clinical presentation, prognosis, and management strategy.
Pathophysiology and risk factors
The pathogenesis of JIA involves complex interactions between the environment and the immune system in genetically susceptible individuals. For most patients, genetic susceptibility is determined by major histocompatibility complex loci. These loci contain genes that encode human leukocyte antigen (HLA) proteins. These proteins present antigenic peptides to T cells for identification of self versus non-self. Environmental exposures (eg, infections, antibiotic use) can elicit an autoimmune response in genetically susceptible individuals (ie, those with certain HLA gene alleles), affecting the following:
- Synovium (ie, connective tissue lining the joint capsule): Inflammatory cells (eg, lymphocytes, plasma cells, macrophages) infiltrate the synovium, resulting in tumor-like tissue proliferation (ie, pannus formation) and fluid accumulation that manifests clinically as joint swelling and deformity.
Continue Learning with UWorld
Get the full Juvenile Idiopathic Arthritis article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessFigures
Images