Pleural Effusion
Article Sections
Introduction
The pleural cavity is a potential space between the visceral and parietal pleural layers that normally contains a trace amount of fluid (~20 mL) serving as a lubricant during respiration (Figure 1). A pleural effusion is an abnormal accumulation of fluid in this space caused by a variety of hydrostatic, secretory, or inflammatory processes that disrupt the balance of fluid formation and resorption.
Pathogenesis and classification
Pleural fluid formation is primarily attributed to 4 major mechanisms (Figure 2).
- Hydrostatic pressure gradient (pleural capillary − pleural space): Increased pleural capillary pressure (eg, from left heart failure) drives extravasation into the pleural space. Fluid builds up until it tamponades further formation (ie, higher left-sided filling pressures lead to larger effusions).
- Oncotic pressure gradient (plasma proteins − pleural fluid proteins): Decreased plasma oncotic pressure (eg, nephrotic syndrome) weakens the colloid drag that pulls fluid back into vessels. However, plasma hypoproteinemia alone cannot induce an effusion. Instead, it plays a minor role in maintaining effusions due to primary disease states associated with hypoalbuminemia (eg, renin-angiotensin-system–induced salt-water retention with nephrotic syndrome and cirrhosis, systemic inflammation and vascular permeability with malignancy and malnutrition).
Continue Learning with UWorld
Get the full Pleural Effusion article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessFigures
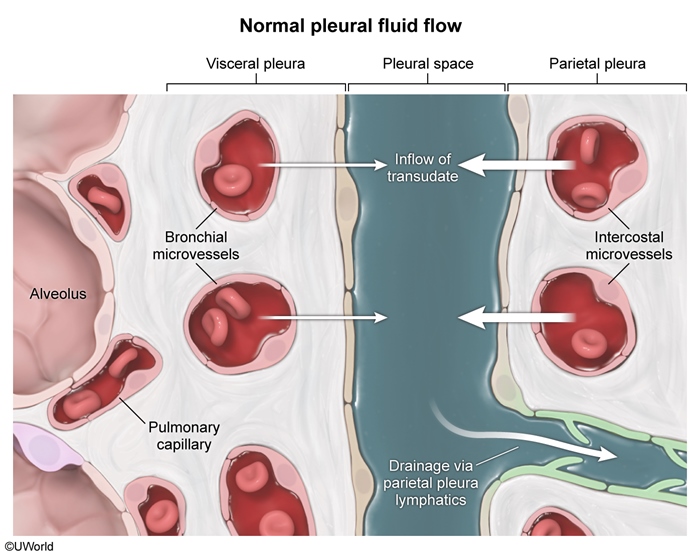
Figure 1
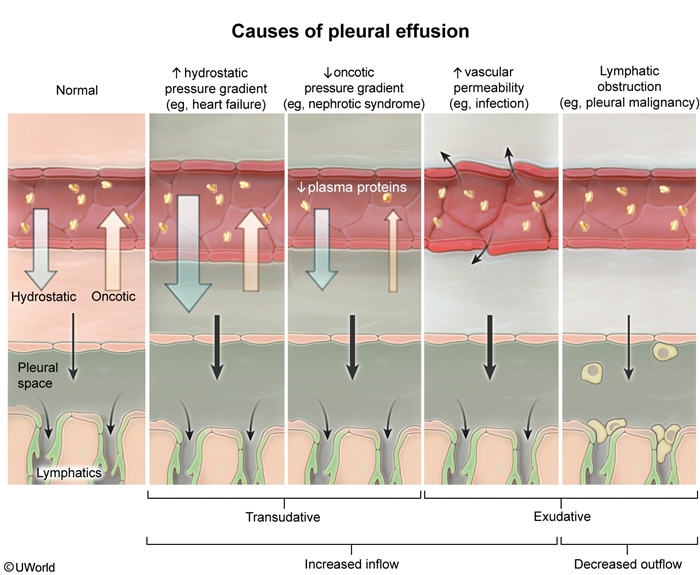
Figure 2
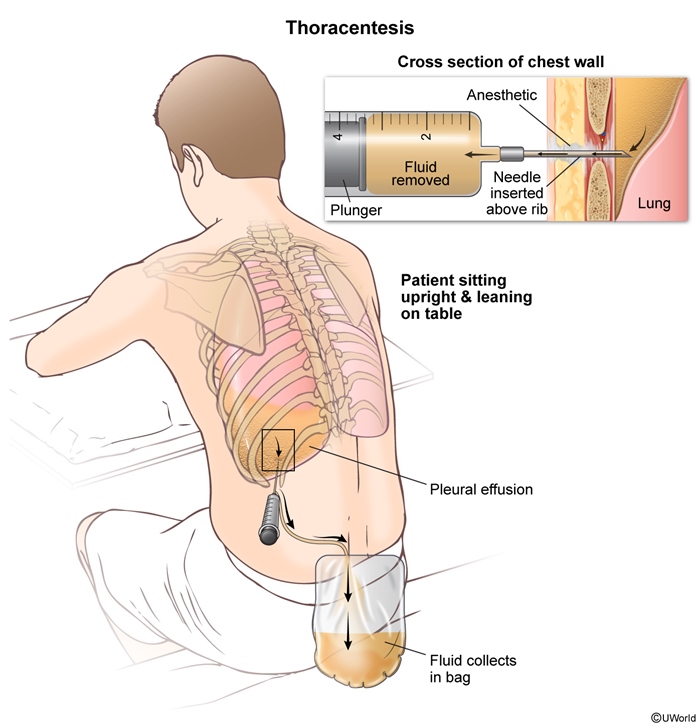
Figure 3
Images
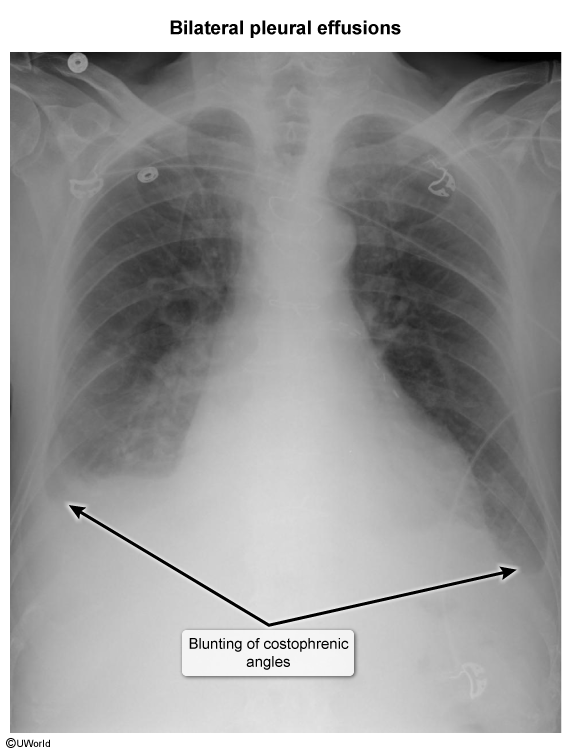
Image 1
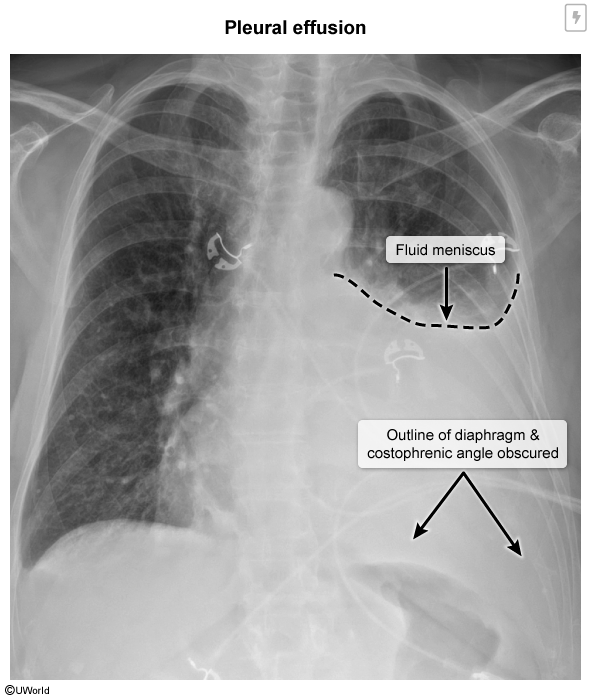
Image 2
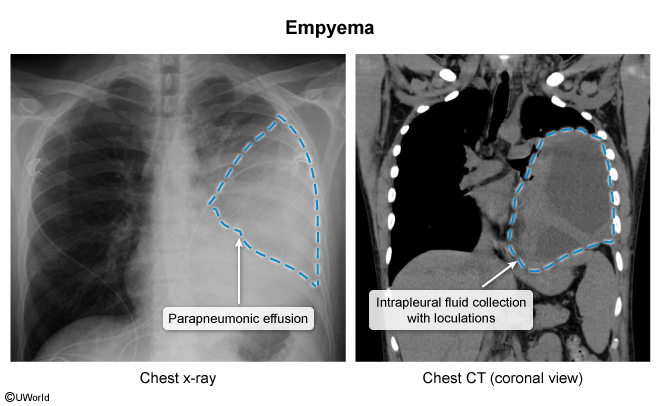
Image 3