Chronic Kidney Disease: An Overview
Article Sections
Introduction
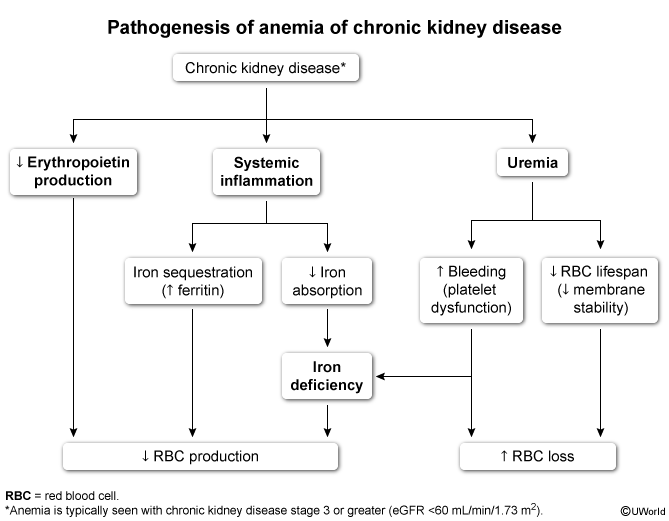
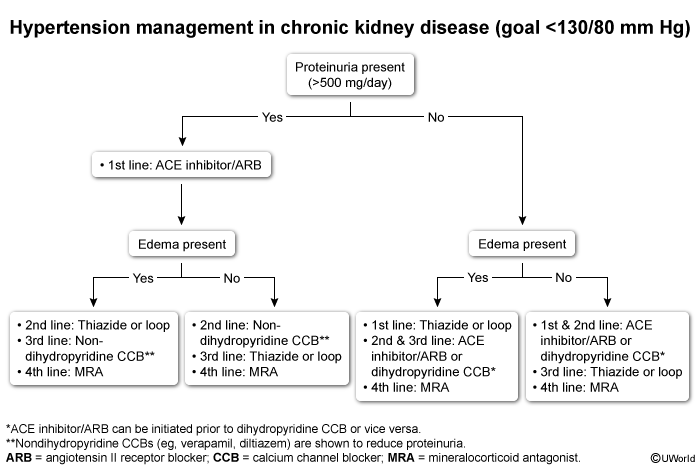
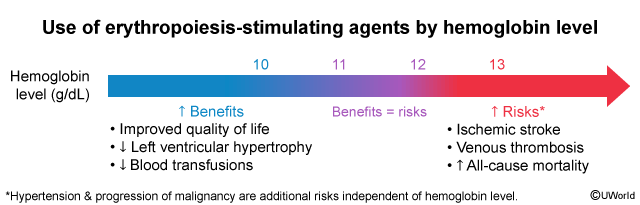
The kidneys are responsible for filtering waste products from the blood, maintaining fluid and electrolyte balance, regulating blood pressure (BP), and producing hormones (eg, erythropoietin). These functions can be disrupted in patients with acute kidney injury (AKI) or chronic kidney disease (CKD).
AKI involves a sudden, often reversible, decline in renal function (discussed in a separate article). CKD is characterized by a progressive, irreversible deterioration of kidney function over months or years. As kidney function declines, waste products accumulate in the blood, leading to a condition known as uremia. CKD is a global health issue affecting a tenth of the world's population and is a major cause of cardiovascular morbidity and mortality.
Pathophysiology
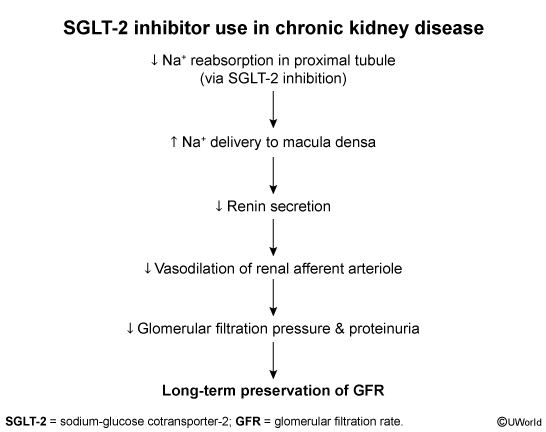
CKD involves a multitude of factors leading to nephron loss with a gradual decline in kidney function. The kidneys initially respond to injury with compensatory mechanisms to maintain the glomerular filtration rate (GFR). These mechanisms include hyperfiltration and hypertrophy of the remaining nephrons, temporarily sustaining kidney function. However, these adaptive responses come at a cost, as the increased pressure and workload on the remaining nephrons eventually lead to further structural and functional damage (eg, glomerulosclerosis, interstitial fibrosis).
Continue Learning with UWorld
Get the full Chronic Kidney Disease: An Overview article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessFigures