Necrotizing Fasciitis
Article Sections
Introduction
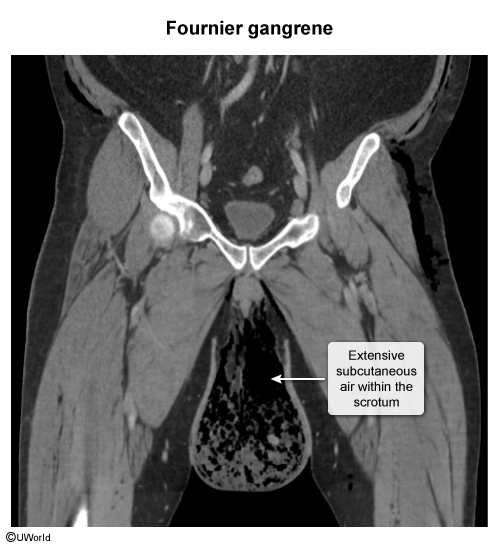
Necrotizing fasciitis is a severe, rapidly progressing infection that results in the destruction of fascia and adjacent soft tissue. It most commonly affects the extremities but can also present as perineal necrotizing fasciitis (Fournier gangrene).
Pathophysiology
Necrotizing fasciitis is triggered by bacteria that invade through minor breaks in the skin, rapidly multiplying and releasing toxins that kill tissue and reduce blood flow, enabling the infection to swiftly spread along fascial planes. Gas production by microbes leads to air in the soft tissues, which results in crepitus on examination in about 50% of cases. Infection initially spreads along the muscle fascia due to its poor blood supply before involving subcutaneous fat. As a result, early identification is difficult.
Histologically, necrotizing fasciitis involves widespread necrosis of subcutaneous tissue and fascia, typically sparing the muscle in its early stages. It features thrombosis of subcutaneous vessels and dense neutrophil infiltration.
Continue Learning with UWorld
Get the full Necrotizing Fasciitis article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessImages