Thrombotic Microangiopathies: Thrombotic Thrombocytopenic Purpura (TTP) And Hemolytic Uremic Syndrome (HUS)
Article Sections
Introduction
Thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) are thrombotic microangiopathies (TMAs) characterized by:
- Microangiopathic hemolytic anemia (MAHA).
- Thrombocytopenia.
- End-organ dysfunction due to microvascular thrombosis.
These high-morbidity and mortality conditions have shared clinical characteristics but differ in terms of pathogenesis, clinical presentation, and management.
Pathophysiology
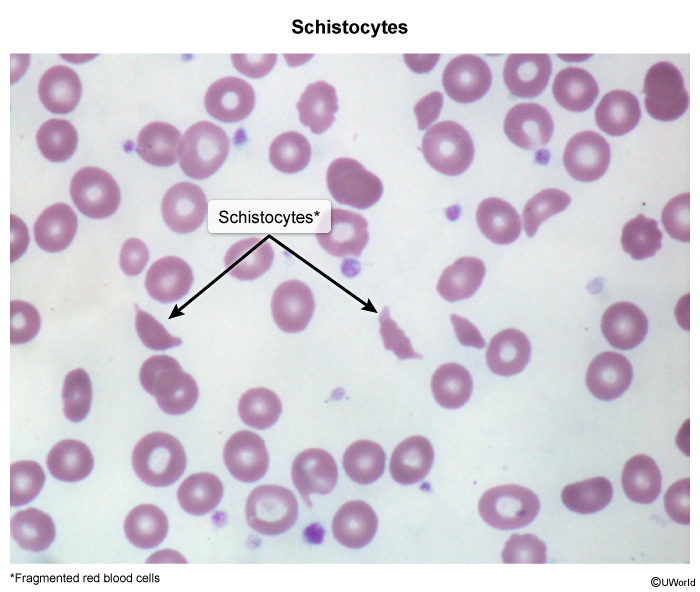
With TMAs, abnormalities in the vessel wall of arterioles result in microthrombus formation. This results in MAHA, which is characterized by anemia from mechanical shearing of red blood cells (RBCs). In TTP and HUS, this shearing occurs as RBCs pass through the microthrombi, producing schistocytes (Image 1).
Thrombotic thrombocytopenic purpuraThere are 2 types of TTP: immune (ie, acquired) and hereditary.
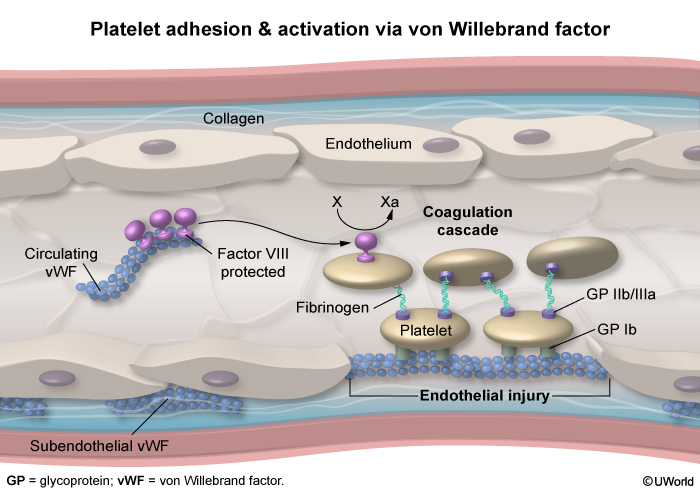
- Acquired TTP occurs due to the formation of an autoantibody against ADAMTS13, a metalloprotease that cleaves von Willebrand factor (vWF) multimers on the endothelial surface (
Continue Learning with UWorld
Get the full Thrombotic Microangiopathies: Thrombotic Thrombocytopenic Purpura (TTP) And Hemolytic Uremic Syndrome (HUS) article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessFigures
Images