Rhinitis
Article Sections
Introduction
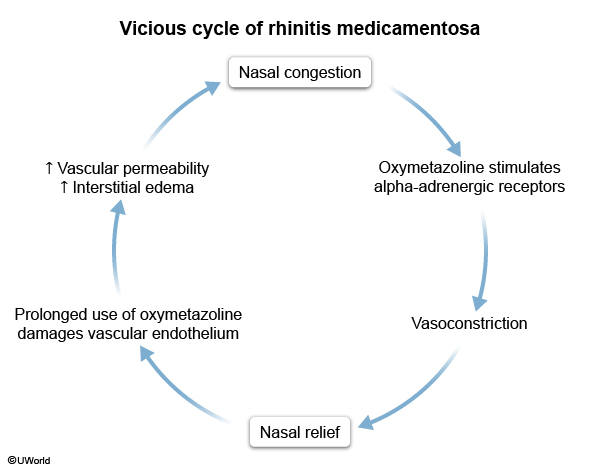
Rhinitis is a common condition that represents a spectrum of inflammatory disorders affecting the nasal mucosa. Patients often have nasal congestion, rhinorrhea, sneezing, and postnasal drip that can impact quality of life. This article focuses on allergic rhinitis, nonallergic rhinitis, and rhinitis medicamentosa.
Pathophysiology
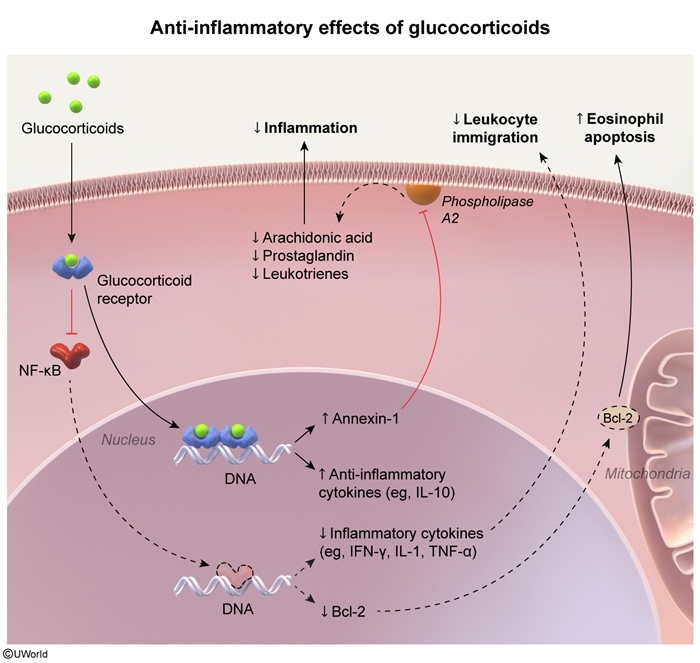
The core mechanism underlying all forms of rhinitis involves inflammation of the nasal mucosa. However, the specific triggers and mediators differ:
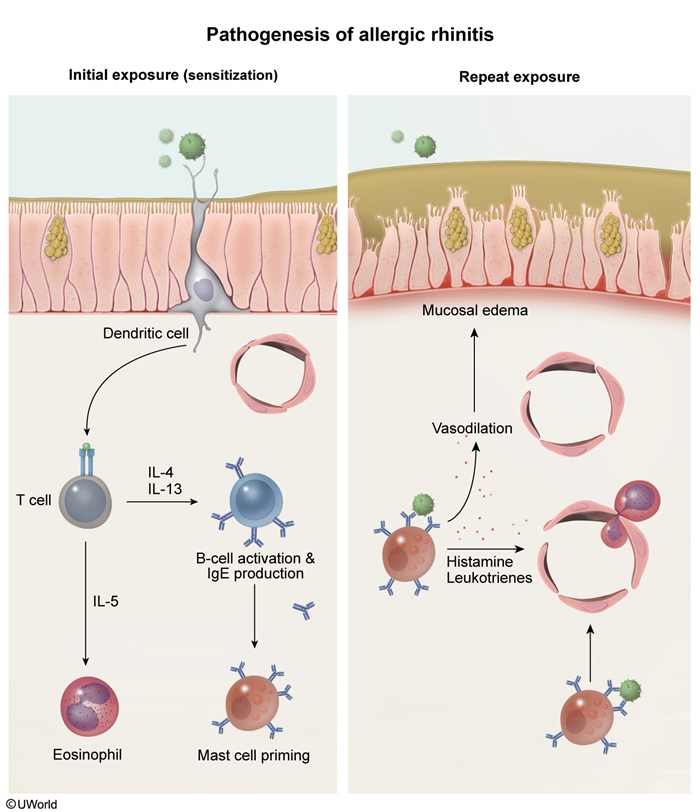
Allergic rhinitisDevelopment of allergic rhinitis is a 2-step process:
-
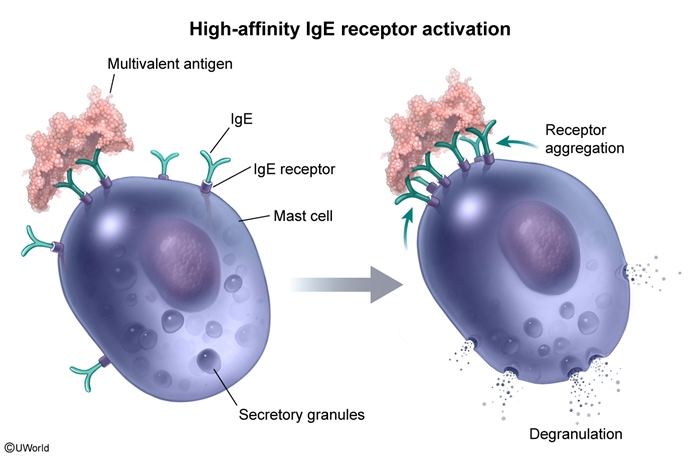
Sensitization occurs when inhaled antigens penetrate the nasal epithelium and are presented on major histocompatibility complex (MHC) class II molecules, causing activation of naive T-helper (Th) cells. The release of cytokines (eg, IL-25, IL-33) from the nasal epithelium promotes Th2-cell differentiation, resulting in secretion of IL-4, IL-13, and other lymphokines that stimulate B-cell maturation and production of IgE antibodies. Antigen-specific IgE antibodies then bind to the high-affinity IgE receptor on mast cells, priming the patient for an allergic response.
Continue Learning with UWorld
Get the full Rhinitis article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessFigures