DRESS Syndrome
Article Sections
Introduction
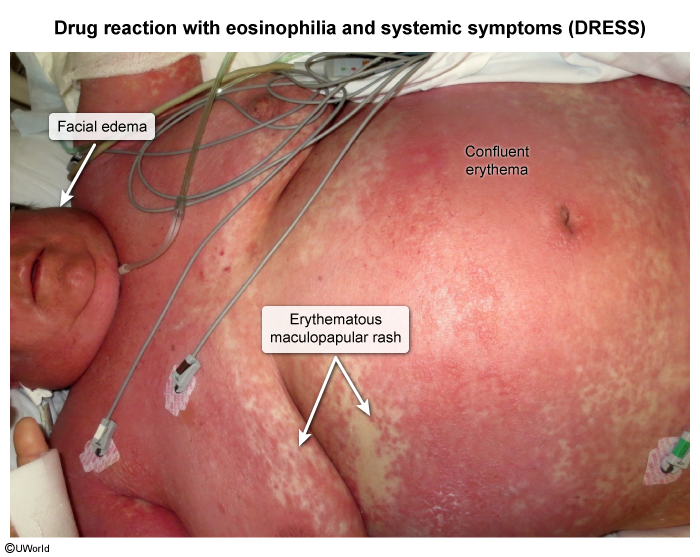
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a potentially life-threatening drug hypersensitivity reaction that occurs 2-8 weeks after exposure. Characteristic clinical findings include a diffuse, erythematous skin rash, fever, facial swelling, lymphadenopathy, eosinophilia, and visceral organ dysfunction. The diagnosis is largely clinical; treatment involves the immediate cessation of the inciting drug and supportive care (eg, fluids). Most patients recover completely within weeks or months, but relapses may occur.
Pathogenesis
DRESS syndrome is a delayed T cell–mediated hypersensitivity reaction commonly associated with medications such as antiepileptics (eg, phenytoin), antibiotics (eg, minocycline), and allopurinol. Unlike other drug reactions, DRESS syndrome has an unusually long latency (2-8 weeks) between drug initiation and the manifestation of symptoms.
The exact pathogenesis is unclear but likely involves a combination of metabolic, genetic, and immunologic factors that cause activation of drug-specific T lymphocytes. These activated T cells release proinflammatory cytokines (eg, tumor necrosis factor alpha), which trigger a robust immune response that leads to inflammation, tissue injury, and necrosis across multiple organ systems, including the skin, liver, kidneys, lungs, and heart.
Continue Learning with UWorld
Get the full DRESS Syndrome article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessImages