Chronic Granulomatous Disease
Article Sections
Introduction
Chronic granulomatous disease (CGD) is a rare primary immunodeficiency disorder of phagocytic metabolism characterized by phagocytes (eg, neutrophils) with impaired NADPH oxidase activity. Patients are at risk for severe, recurrent bacterial and fungal infections and granuloma formation.
Pathogenesis
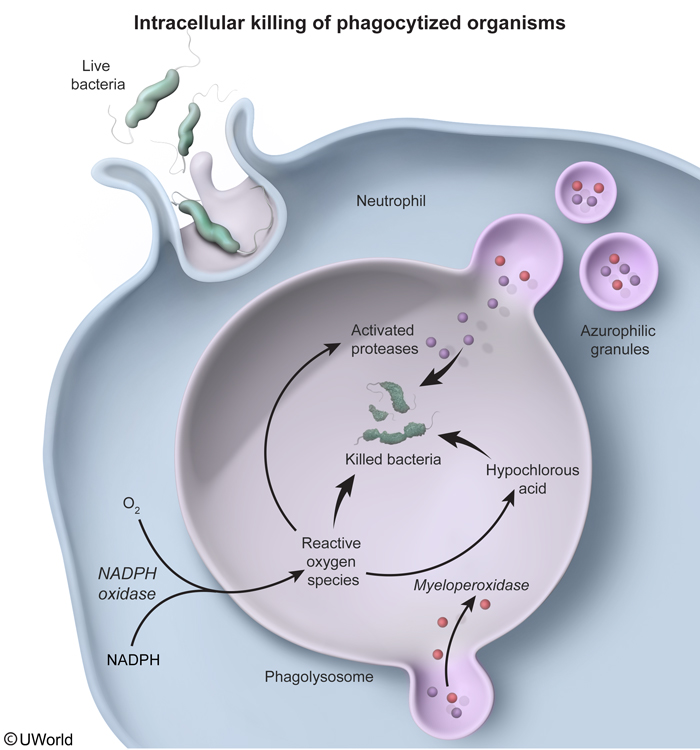
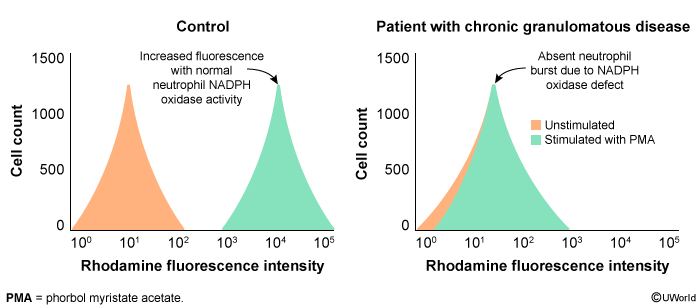
CGD most commonly occurs due to an X-linked recessive mutation in the gene that encodes NADPH oxidase, a membrane-bound enzyme complex that catalyzes the reduction of oxygen to reactive oxygen species (ROS) (eg, superoxide, hydrogen peroxide) during the respiratory burst (Figure 1). ROS activate granule proteases that kill phagocytosed pathogens within the phagolysosome.
Without NADPH oxidase, patients with CGD have an impaired respiratory burst. Although protease degranulation occurs normally, these proteases are not activated due to the absence of ROS, resulting in defective phagocytic intracellular killing. The defective phagocytes in patients with CGD can still kill many pathogens because most microorganisms naturally produce hydrogen peroxide as a byproduct of metabolism, which can activate granule proteases. However, catalase-positive bacteria and fungi are pathogenic in CGD because they degrade their own metabolically produced hydrogen peroxide (an ROS), further limiting microbicidal protease activation. Therefore, patients with CGD are susceptible to infections by catalase-positive organisms, particularly:
Continue Learning with UWorld
Get the full Chronic Granulomatous Disease article plus rich visuals, real-world cases, and in-depth insights from medical experts, all available through the UWorld Medical Library.
Unlock Full AccessFigures